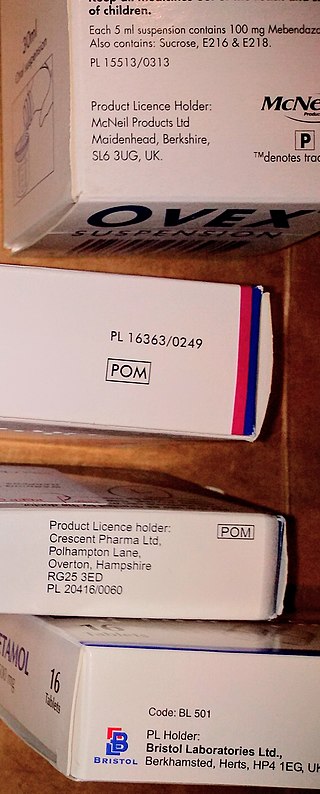
The British National Formulary (BNF) is a United Kingdom (UK) pharmaceutical reference book that contains a wide spectrum of information and advice on prescribing and pharmacology, along with specific facts and details about many medicines available on the UK National Health Service (NHS). Information within the BNF includes indication(s), contraindications, side effects, doses, legal classification, names and prices of available proprietary and generic formulations, and any other notable points. Though it is a national formulary, it nevertheless also includes entries for some medicines which are not available under the NHS, and must be prescribed and/or purchased privately. A symbol clearly denotes such drugs in their entry.

A medication is a drug used to diagnose, cure, treat, or prevent disease. Drug therapy (pharmacotherapy) is an important part of the medical field and relies on the science of pharmacology for continual advancement and on pharmacy for appropriate management.
Prescription drug list prices in the United States continually rank among the highest in the world. The high cost of prescription drugs became a major topic of discussion in the 21st century, leading up to the American health care reform debate of 2009, and received renewed attention in 2015. One major reason for high prescription drug prices in the United States relative to other countries is the inability of government-granted monopolies in the American health care sector to use their bargaining power to negotiate lower prices and that the American payer ends up subsidizing the world's R&D spending on drugs.
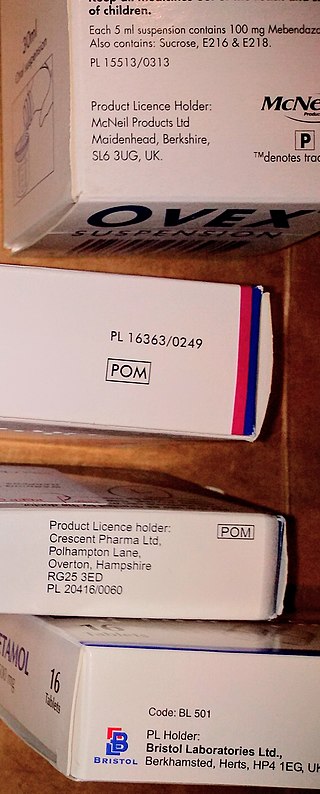
A prescription drug is a pharmaceutical drug that is only permitted to be dispensed to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.
The pregnancy category of a medication is an assessment of the risk of fetal injury due to the pharmaceutical, if it is used as directed by the mother during pregnancy. It does not include any risks conferred by pharmaceutical agents or their metabolites in breast milk.
The Pharmaceutical Benefits Scheme (PBS) is a program of the Australian Government that subsidises prescription medication for Australian citizens and permanent residents, as well as international visitors covered by a reciprocal health care agreement. The PBS is separate to the Medicare Benefits Schedule, a list of health care services that can be claimed under Medicare, Australia's universal health care insurance scheme.
Many countries have measures in place to limit advertising by pharmaceutical companies.

BNF for Children (BNFC) is the standard UK paediatric reference for prescribing and pharmacology.
Senaka Bibile was a Sri Lankan pharmacologist. He was the founder of Sri Lanka's drug policy, which was used as a model for development of policies based on rational pharmaceutical use in other countries as well by the World Health Organization, the United Nations Conference on Trade and Development (UNCTAD) and the Non-Aligned Movement. Due to the far reaching effects of his proposals and policies, he has been called the 'greatest medical benefactor of humanity that Sri Lanka has hitherto produced'.
The Sri Lanka National Pharmaceuticals Policy was established in the 1970s following the submission of a report by Dr S.A. Wickremasinghe and Prof. Seneka Bibile. It aimed at ensuring that people get good quality drugs at the lowest possible price and that doctors would prescribe the minimum required drugs to treat the patient's illness. It was a pioneer in the field of rational National pharmaceuticals policy.
The National Medicinal Drugs Policy is an essential part of Sri Lanka's Health Policy, aimed at the rational use of pharmaceuticals.

The State Pharmaceuticals Corporation (SPC) is a state-owned enterprise with its headquarters in Colombo, Sri Lanka. It is the largest supplier of drugs in the country, and is tasked with providing quality-assured health care items that are safe and effective, at an affordable price, while educating the public on the rational use of drugs. It employees about 600 staff.
In the United States, a pharmacy benefit manager (PBM) is a third-party administrator of prescription drug programs for commercial health plans, self-insured employer plans, Medicare Part D plans, the Federal Employees Health Benefits Program, and state government employee plans. According to the American Pharmacists Association, "PBMs are primarily responsible for developing and maintaining the formulary, contracting with pharmacies, negotiating discounts and rebates with drug manufacturers, and processing and paying prescription drug claims." PBMs operate inside of integrated healthcare systems, as part of retail pharmacies, and as part of insurance companies.
Many developing nations have developed national drug policies, a concept that has been actively promoted by the WHO. For example, the national drug policy for Indonesia drawn up in 1983 had the following objectives:
Pharmaceutical policy is a branch of health policy that deals with the development, provision and use of medications within a health care system. It embraces drugs, biologics, vaccines and natural health products.

A pharmacy is a retail shop which provides pharmaceutical drugs, among other products. At the pharmacy, a pharmacist oversees the fulfillment of medical prescriptions and is available to counsel patients about prescription and over-the-counter drugs or about health problems and wellness issues. A typical pharmacy would be in the commercial area of a community.
Medication costs, also known as drug costs are a common health care cost for many people and health care systems. Prescription costs are the costs to the end consumer. Medication costs are influenced by multiple factors such as patents, stakeholder influence, and marketing expenses. A number of countries including Canada, parts of Europe, and Brazil use external reference pricing as a means to compare drug prices and to determine a base price for a particular medication. Other countries use pharmacoeconomics, which looks at the cost/benefit of a product in terms of quality of life, alternative treatments, and cost reduction or avoidance in other parts of the health care system. Structures like the UK's National Institute for Health and Clinical Excellence and to a lesser extent Canada's Common Drug Review evaluate products in this way.
A formulary is a list of pharmaceutical drugs, often decided upon by a group of people, for various reasons such as insurance coverage or use at a medical facility. Traditionally, a formulary contained a collection of formulas for the compounding and testing of medication. Today, the main function of a prescription formulary is to specify particular medications that are approved to be prescribed at a particular hospital, in a particular health system, or under a particular health insurance policy. The development of prescription formularies is based on evaluations of efficacy, safety, and cost-effectiveness of drugs.
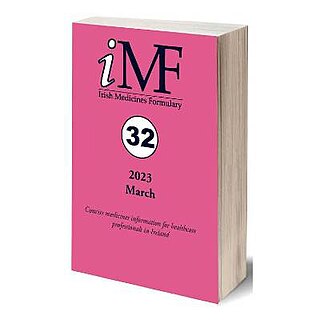
Irish Medicines Formulary (IMF) is a medicines reference for doctors, nurses, pharmacists and dentists, providing medicines information which is medico-legally relevant in Ireland. It is published in online and print formats, and lists original brands, branded generics and pure generic prescription medicines.
The Top 100 Drugs: Clinical Pharmacology and Practical Prescribing is a pocket-size medical manual focusing on the most commonly prescribed medicines by the British National Health Service (NHS). It was first published by Churchill Livingstone, Elsevier, in 2014, and revised in a second edition in 2018. It is authored by four clinical pharmacologists from St George's Hospital, London; Andrew Hitchings, Dagan Lonsdale, Daniel Burrage and Emma Baker.