History of Women's Health in China
| Part of a series on |
| Women's health |
|---|
| |
Late Qing dynasty
In the late 19th century, Chinese reformers began call for the modernization of childbirth based on Western scientific medicine. [3] : 104 These debates intensified when May Fourth Movement reformers began criticizing the role of the traditional midwife for what they described as its backwardness and feudal superstition. [3] : 104
Nationalist China
In the 1920s, the Nationalist government drafted a national program of maternal and infant health care which built off the ideas of the May Fourth reformers and other concepts of medical modernization which were developing around the world. [3] : 104
China lacked medical infrastructure and modern-style medical personnel, and the Nationalist program therefore focused on professionalizing midwifery with different regulations for rural and urban areas. [3] : 104–105
Pre-reform PRC (1949-1978)
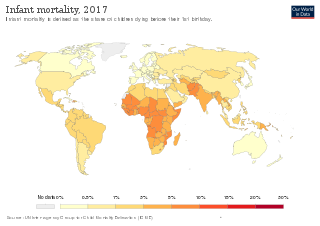
After the 1949 founding of the People's Republic of China, the country established its first public healthcare system, the Cooperative Medical Scheme (CMS), which focused on the needs of the country's huge rural population. [4] The CMS was a three-tier system: barefoot doctors, township health centers, and country hospitals. In the end of the 1970s, over 90% of rural villages had set up cooperative medical schemes (CMS). [5] The implementation of CMS has seen significant improvement in population health in China, including female health. [6] Studies by Mei-yu Yu et al. found that the female Infant Mortality Rate (IMR) declined from 170 per 1000 in 1953 to 136 in 1957, and female average life expectancy at birth rose from 44.8 in 1949 to 67.1 in 1975. [2] Contrary to the Chinese census, Banister's studies have shown that female IMR is higher than male IMR in China at least since 1975. [7] Mei Yu-yu et al. believed that such a discrepancy in IMR between female and male could be a result of preference for sons in traditional Chinese ideology, which may cause abandonment, unequal treatment or violence against female infants. [2]
In the PRC's early years, traditional midwives came to be viewed as dirty and unscientific. [8] The government sought to expand hospital infrastructure and to replace traditional midwifery with modern techniques approved by the newly-established socialist health authorities. [3] : 105 In urban areas, women increasingly gave birth at hospitals. [3] : 105 In rural areas, women continued to give birth with the aid of local midwives, including those certified by the government who had taken a short-term course on new birthing methods. [3] : 105 By 1959, over 750,000 midwives were retrained with some modern medical practice, but only 5,300 were fully modern trained midwives. [9] With China's program of barefoot doctors, perinatal practitioners were often older women. [10] Their work was effective, with much of the 1950s and 1960s population boom resulting from the decline in infant mortality. [10]
By the late 1970s, most rural areas had a developed but low-tech childbirth infrastructure, with local teams of certified lay midwives worker with barefoot doctors. [3] : 105 Rates of hospital births increased significantly in China as a whole, with most home births occurring in rural areas. [3] : 105
Economic reform (1979–present)
During Reform and Opening Up, China implemented far-reaching reforms: decollectivization and land tenure reforms, promotion of township and village enterprises (TVEs), state sector reforms, and policies to encourage foreign direct investment (FDI) and trade liberalization. These policies were implemented as China moved to a market economy and were furthered in order to insure their membership to the World Trade Organization (WTO). [5] These policies are hailed by many as being highly successful, producing massive economic growth while raising the standard of living by reducing poverty. China has taken a gradual and highly regulated approach to its transformation, and while China started its transformation earlier than other socialist countries. it is still undergoing that transformation. These measures have led to much growth, and as China continues to increase its GDP, those same policies have led to decentralization and privatization of healthcare. [5]
In the 1980s, the necessity of rural home births continued to be reflected in health care regulations. [3] : 106
Beginning in the 1990s, the China received significant foreign aid to improve its hospital and medication equipment, in part due to major international public health campaigns like the United Nations Safe Motherhood Initiative and the Millennium Development Goals Program. [3] : 106 China also allowed public hospitals to finance technological upgrades through fees charged to patients. [3] : 106
Hospitals births were made compulsory. [3] : 106–107
Health and dormitory life
As the market opened new employment, opportunities for women became available. Those new opportunities were primarily in the service and textile industries. The number of Chinese women working as of 2007 was 330 million which is now 46.7% of the total working population, the majority of these women are working in the agricultural or industrial sectors with a high concentration working in the garment industry. [11] These industries lend themselves to dormitory living. These dormitories are filled with migrant workers, none of whom can stay in the urban areas without being employed. [12] Young women have become the most prevalent demographic for migrant work, making up over 70% of those employed in the garment, toy, and electronic industries. [12] These women now called dagongmei are typically short term laborers who are contracted for a short period of time and at the end of their contracts they either find more work or are forced to return home. That type of labor contract leaves these dagongmei with very little bargaining power as they seem to be easily replaceable.[ citation needed ]
The dormitory life in China leaves women with little to no home space independence from the factory. All of the women's time spent traveling from home to work is eliminated and working days are extended to suit production needs. [12] Sick days and personal health are of little concern in these dormitory settings. Women will often neglect their own health out of fear of retribution from factory supervisors. Furthermore, as shown in the documentary "China Blue" if a woman becomes pregnant while working she will be either fired or forced to quit shortly after her baby is born because she will not be able to meet her work responsibilities. In 2009 alone, over 20,000 Chinese dorm workers became ill while living in these dorms, the majority being young women. While living in dormitories, women migrant workers' time is not their own. As they become assimilated into the factory life they are almost completely controlled by the paternalistic systems of these factory owners and managers. Hygiene and communicable diseases become a threat to health as women live in rooms of 8-20 people sharing washrooms between rooms and floors of the dormitories. The only private space allotted is behind the curtain that covers an individual's bunk. Male and female workers are separated and there are strict controls placed on the sexual activity of both. These conditions pose a great threat to not only the physical but also the mental health of these women workers being away from their home and placed in a highly restrictive environment. [12] While those changes did allow China to achieve unprecedented economic growth, the privatization of many industries also forced China to reform its healthcare policies.[ citation needed ]
Wage discrimination reduces access to healthcare
Another factor that limits women's capabilities to access healthcare is their relative low wage compared to men. China promotes itself as having almost no gender bias when it comes to wages yet we see that compared to men women are making less money. The Chinese government touts their "equal pay for equal work" mantra, however, women find that their work in the textile industries is not equal to the work done in industries requiring "heavy" labor so in the end women make less than men because they are perceived as not being able to do the "heavy" work. [13] This inequitable pay leaves women more vulnerable and with less capability to pay for their individual healthcare when compared to men. While 49.6% of women are uninsured demonstrating that there is not much disparity between uninsured men and women. [14] The lack of insurance does not affect men and women equally as women needs tend to be greater in order to provide care for child birth, family care, and security. [14] Social security coverage has also been a factor as only 37.9% of those receiving social security are women; again this becomes an issue as elderly women are unable to pay for their growing health costs. As the cost of healthcare increases due to deregulation of trade and privatization, research has shown that the conditions mentioned above have greatly reduced women's capability to access healthcare in China. [14]
WTO membership (2001-present)
While China's entry to WTO was presumed to further motivate its economic development and improve its market structure, it has also been worried that joining WTO will worsen China's labor surplus because over-hired labor in state enterprises [15] may be deemed "inefficient" once China entered global market. Moreover, studies have shown that the workforce in China was made of only 40% women but 60% of those laid off were women, which demonstrated that women are much more vulnerable to these effects than man. [16]
Statistics obtained in 2008 have shown that males enjoy higher physical well-being than females. However, it is not addressed if the situation could be related to China's changing economy in any ways. [17]
By the 2010s, the practice of home birth had ended through the practice of subsidizing rural hospital deliveries and banning rural midwives from practicing. [3] : 107