Mpox is an infectious viral disease that can occur in humans and other animals. Symptoms include a rash that forms blisters and then crusts over, fever, and swollen lymph nodes. The illness is usually mild and most of those infected will recover within a few weeks without treatment. The time from exposure to onset of symptoms ranges from five to twenty-one days and symptoms typically last from two to four weeks. Cases may be severe, especially in children, pregnant women or people with suppressed immune systems.

The 1972 Yugoslav smallpox outbreak was the largest outbreak of smallpox in Europe after the Second World War. It was centered in SAP Kosovo, a province of Serbia within Yugoslavia, and the capital city of Belgrade. A Kosovar Albanian Muslim pilgrim had contracted the smallpox virus in the Middle East. Upon returning to his home in Kosovo, he started the epidemic in which 175 people were infected, killing 35. The epidemic was efficiently contained by enforced quarantine and mass vaccination. The 1982 film Variola Vera is based on the event.

The New World of the Western Hemisphere was devastated by the 1775–1782 North American smallpox epidemic. Estimates based on remnant settlements say at least 130,000 people were estimated to have died in the epidemic that started in 1775.
Orthopoxvirus is a genus of viruses in the family Poxviridae and subfamily Chordopoxvirinae. Vertebrates, including mammals and humans, and arthropods serve as natural hosts. There are 12 species in this genus. Diseases associated with this genus include smallpox, cowpox, horsepox, camelpox, and mpox. The most widely known member of the genus is Variola virus, which causes smallpox. It was eradicated globally by 1977, through the use of Vaccinia virus as a vaccine. The most recently described species is the Alaskapox virus, first isolated in 2015.

Ali Maow Maalin was a Somali hospital cook and health worker from Merca who is the last person known to have been infected with naturally occurring Variola minor smallpox. He was diagnosed with the disease in October 1977 and made a full recovery. Although he had many contacts, none of them developed the disease, and an aggressive containment campaign was successful in preventing an outbreak. Smallpox was declared to have been eradicated globally by the World Health Organization (WHO) two years later. Maalin was subsequently involved in the successful poliomyelitis eradication campaign in Somalia, and he died of malaria while carrying out polio vaccinations after the re-emergence of the poliovirus in 2013.
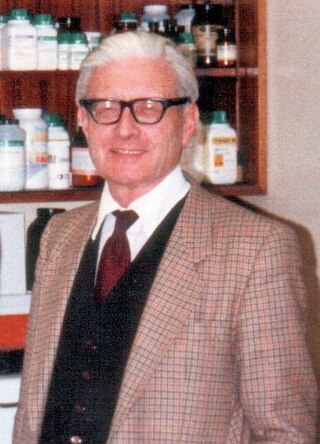
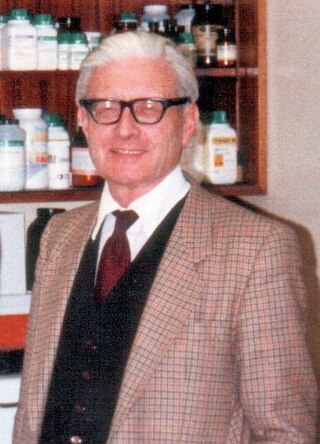
Thomas Henry Flewett, MD, FRCPath, FRCP was a founder member of the Royal College of Pathologists and was elected a Fellow of the Royal College of Physicians of London in 1978. He was chairman of the World Health Organization (WHO) Steering Committee on Viral Diarrhoeal Diseases, 1990–3, and a member until 1996. His laboratory in Birmingham was a World Health Organization Reference and Research Centre for Rotavirus Infections from 1980 until his retirement in 1987. He was an external examiner, visiting lecturer, and scientific journal editor. He was a member of the board of the Public Health Laboratory Service from 1977 to 1983 and was chairman of the Public Health Laboratory Service's Committee on Electron Microscopy from 1977 to 1987.

Variola Vera is a 1982 Yugoslav film directed by Goran Marković.

Smallpox was an infectious disease caused by variola virus, which belongs to the genus Orthopoxvirus. The last naturally occurring case was diagnosed in October 1977, and the World Health Organization (WHO) certified the global eradication of the disease in 1980, making smallpox the only human disease to have been eradicated to date.

The social history of viruses describes the influence of viruses and viral infections on human history. Epidemics caused by viruses began when human behaviour changed during the Neolithic period, around 12,000 years ago, when humans developed more densely populated agricultural communities. This allowed viruses to spread rapidly and subsequently to become endemic. Viruses of plants and livestock also increased, and as humans became dependent on agriculture and farming, diseases such as potyviruses of potatoes and rinderpest of cattle had devastating consequences.
The Massachusetts smallpox epidemic or colonial epidemic was a smallpox outbreak that hit Massachusetts in 1633. Smallpox outbreaks were not confined to 1633 however, and occurred nearly every ten years. Smallpox was caused by two different types of variola viruses: variola major and variola minor. The disease was hypothesized to be transmitted due to an increase in the immigration of European settlers to the region who brought Old World smallpox aboard their ships.

Brincidofovir, sold under the brand name Tembexa, is an antiviral drug used to treat smallpox. Brincidofovir is a prodrug of cidofovir. Conjugated to a lipid, the compound is designed to release cidofovir intracellularly, allowing for higher intracellular and lower plasma concentrations of cidofovir, effectively increasing its activity against dsDNA viruses, as well as oral bioavailability.
The smallpox virus retention debate has been going on among scientists and health officials since the smallpox virus was declared eradicated by the World Health Organization (WHO) in 1980. The debate centers on whether or not the last two known remnants of the Variola virus known to cause smallpox, which are kept in tightly controlled government laboratories in the United States and Russia, should be finally and irreversibly destroyed. Advocates of final destruction maintain that there is no longer any valid rationale for retaining the samples, which pose the hazard of escaping the laboratories, while opponents of destruction maintain that the samples may still be of value to scientific research, especially since variants of the smallpox virus may still exist in the natural world and thus present the possibility of the disease re-emerging in the future or being used as a bio-weapon.
Catherine-de-Barnes Isolation Hospital was a specialist isolation hospital for infection control in Catherine-de-Barnes, a village within the Metropolitan Borough of Solihull in the English county of West Midlands.
Witton Isolation Hospital was a facility for the treatment and quarantine of smallpox victims and their contacts in Birmingham, England, from 1894 to 1966.

An outbreak of smallpox in Bradford in 1962 first came to attention on 11 January 1962, when a cook from the children's hospital in Bradford, West Riding of Yorkshire, England, presented with an unexplained fever and was found to have changes in her blood similar to another sick person at the nearby St Luke's Hospital, both samples appearing compatible with smallpox. The index case was later discovered to be a nine-year old girl who arrived in the UK on 16 December 1961 from Karachi, Pakistan, where there was an ongoing epidemic of smallpox.

Henry Samuel Bedson, MD, MRCP, was a British virologist and head of the Department of Medical Microbiology at Birmingham Medical School, where his research focused on smallpox and monkeypox virus.
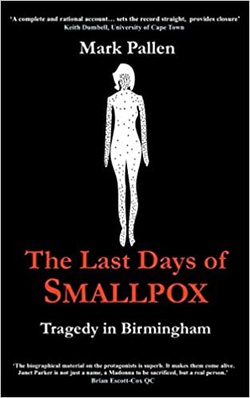
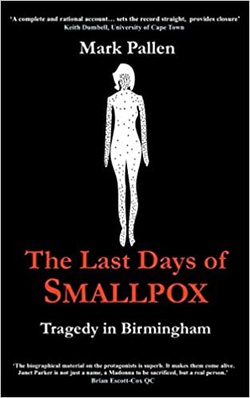
The Last Days of Smallpox: Tragedy in Birmingham is a 2018 nonfiction account of the events leading up to and following the 1978 smallpox outbreak in the United Kingdom. The author, Mark Pallen, proposes an explanation of how Janet Parker – the last person to die from smallpox – contracted the infection. This explanation, based on court transcripts and interviews with the barrister who defended the University, and the clinicians and scientists who were involved with the outbreak, contradicts the conclusions of the official government enquiry, The Shooter Report.
Alasdair Macintosh Geddes was a British medical doctor who was Professor of Infection at the University of Birmingham Medical School. In 1978, as the World Health Organization (WHO) was shortly to announce that the world's last case of smallpox had occurred a year earlier in Somalia, Geddes diagnosed a British woman with the disease in Birmingham, England. She was found to be the index case of the outbreak and became the world's last reported fatality due to the disease, five years after he had gained experience on the frontline of the WHO's smallpox eradication programme in Bangladesh in 1973.

Lucas Alfred Derrick Tovey FRCPath, FRCOG, was a British pathologist who shortly after being appointed consultant at St Luke's Hospital in Bradford, West Yorkshire, England, recognised the first cases of smallpox in the early days of the Bradford smallpox outbreak of 1962. Over the subsequent three days a further eight cases of smallpox were detected and Tovey subsequently became in charge of infection control at St Luke's and given the responsibility of liaising with the medical officers of health and the press. He later attributed the successful containment of the outbreak to effective contact tracing, surveillance and vaccination.

Surinder Singh Bakhshi is a British writer and physician, who in 1977 was appointed medical officer of environmental health to the Birmingham Area Health Authority, where he led the successful contact tracing and quarantine effort in the community during the 1978 smallpox outbreak in the United Kingdom.