Classification of 3D culture methods
There are a large number of commercially available culturing tools that claim to provide the advantages of 3D cell culture. In general, the platforms can be classified in two types of 3D culturing methods: scaffold techniques and scaffold-free techniques.

Scaffold techniques
Scaffold techniques include the use of solid scaffolds, hydrogels and other materials. In a recent study potentiality of human CD34+ stem cells explored by generating in vitro agarose gel 3D model to understand the bone ossification process. [25] Scaffolds can be used to generate microtissue 3D model by culturing fibroblasts outside of tumour cells, mimicking the tumor stroma interaction. [26]
The effectiveness of scaffolds in various applications, particularly in tissue engineering, is significantly impacted by factors such as pore distribution, exposed surface area, and porosity. The quantity and arrangement of these elements influence both the depth and rate at which cells penetrate the scaffold volume, the structure of the resulting extracellular matrix, and ultimately, the success of the regenerative process. [27] Scaffolds can be produced with diverse architectures depending on the manufacturing method, leading to either random or precisely designed pore distribution. [28] Recently, advanced computer-controlled rapid prototyping techniques have been employed to create scaffolds with well-organized geometries. [29]
Hydrogels
As the natural extracellular matrix (ECM) is important in the survival, proliferation, differentiation and migration of the cells, different hydrogel matrices mimicking natural ECM structure are considered as potential approaches towards in vivo –like cell culturing. [30] [31] [32] Hydrogels are composed of interconnected pores with high water retention, which enables efficient transport of e.g. nutrients and gases. Several different types of hydrogels from natural and synthetic materials are available for 3D cell culture, including e.g. animal ECM extract hydrogels, protein hydrogels, peptide hydrogels, polymer hydrogels, and wood-based nanocellulose hydrogel.
The approach to crafting the optimal ECM replica relies on the specific characteristics of the culture in question and typically involves employing diverse and independent chemical processes. [33] For example, the utilization of photolabile chemistries can lead to the erosion of specific regions within a gel, and subsequently exposing these areas allows for the application of adhesive ligands, promoting cell adhesion and migration. [34] The development of more intricate frameworks is anticipated, comprising interwoven networks of chemistries under the control of both cells and users. In essence, there is no singular network capable of faithfully emulating the intricate ECM of every tissue type. However, a thoughtful integration of bioinspired cues into synthetic gels holds the potential to yield resilient and versatile scaffolds applicable across various cell culture systems. [35]
Scaffold-free techniques
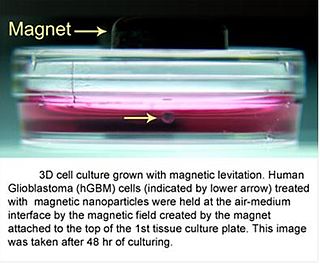
Scaffold free techniques employ another approach independent from the use scaffold. Scaffold-free methods include e.g. the use of low adhesion plates, hanging drop plates, micropatterned surfaces, and rotating bioreactors, magnetic levitation, and magnetic 3D bioprinting.
Spheroids

Spheroids are a type of three-dimensional cell modeling that better simulate a live cell's environmental conditions compared to a two-dimensional cell model, specifically with the reactions between cells and the reactions between cells and the matrix. [37] Spheroids are useful in the study of changing physiological characteristics of cells, [38] the difference in the structure of healthy cells and tumor cells, and the changes cells undergo when forming a tumor. [39] Spheroids co-cultured with tumor and healthy cells were used to simulate how cancerous cells interact with normal cells. [40] Spheroids can also be co-cultured with fibroblasts to mimic tumor-stroma interaction. [41] Spheroids can be grown with a few different methods. One common method is to use low cell adhesion plates, typically a 96 well plate, to mass-produce spheroid cultures, where the aggregates form in the rounded bottom of the cell plates. [36] [42] Spheroids can also be cultured using the hanging drop method [43] involving forming cell aggregates in drops that hang from the surface of a cell plate. [37] Other methods under investigation include the use of rotating wall vessel bioreactors, which spins and cultures the cells when they are constantly in free fall and forms aggregates in layers [44] Recently, some protocols have been standardized to produce uniform and reliable spheroids. [45] Researchers had also explored standardized, economical and reproducible methods for 3D cell culture. [46] To improve reproducibility and transparency in spheroid experiments, an international consortium developed MISpheroID (Minimal Information in Spheroid Identity). [47]
Clusteroids
clusteroids are a type of three-dimensional cell modeling similar to spheroids but are distinguished by their creation method; grown as clusters of cells in an aqueous two-phase system of water-in-water Pickering emulsion using interfacial tension and osmotic shrinkage to pack the cells into dense clusters which are then cultured in a hydrogel into tissues or organoids. [48] [49]
In the absence of blood vessels, oxygen permeability is impaired during necrotic nucleus formation and this prevents the ex vivo use of 3D cell culture. There is an emulsion template that can overcome this problem. This approach allowed researchers to adjust the cell composition to attain the ideal conditions for promoting the synthesis of diverse angiogenic protein markers within the co-cultured clusteroids. [50] HUVEC cells exhibit a reaction to the presence of Hep-G2 cells and their derivatives by generating endothelial cell sprouts in Matrigel, all without the external introduction of vascular endothelial growth factor (VEGF) or other agents that induce angiogenesis. [51] [52] The replication of this cultivation technique is straightforward for generating various cell co-culture spheroids. [53] The w/w Pickering emulsion template greatly aids in constructing 3D co-culture models, offering significant potential for applications in drug testing and tissue engineering. [54]
Bioreactors
The bioreactors used for 3D cell cultures are small plastic cylindrical chambers that are specifically engineered for the purpose of growing cells in three dimensions. The bioreactor uses bioactive synthetic materials such as polyethylene terephthalate membranes to surround the spheroid cells in an environment that maintains high levels of nutrients. [55] [56] They are easy to open and close, so that cell spheroids can be removed for testing, yet the chamber is able to maintain 100% humidity throughout. [1] This humidity is important to achieve maximum cell growth and function. The bioreactor chamber is part of a larger device that rotates to ensure equal cell growth in each direction across three dimensions. [1]
MC2 Biotek has developed a bioreactor to incubate proto-tissue that uses gas exchange to maintain high oxygen levels within the cell chamber. [57] This is an improvement over previous bioreactors because the higher oxygen levels help the cell grow and undergo normal cell respiration. [15]
Collaborative efforts between tissue engineering (TE) firms, academic institutions, and industrial partners can enhance the transformation of research-oriented bioreactors into efficient commercial manufacturing systems. [58] Academic collaborators contribute foundational aspects, while industrial partners provide essential automation elements, ensuring compliance with regulatory standards and user-friendliness. [59] Established consortia in Europe, such as REMEDI, AUTOBONE, and STEPS, focus on developing automated systems to streamline the engineering of autologous cell-based grafts. [60] The aim is to meet regulatory criteria and ensure cost-effectiveness, making tissue-engineered products more clinically accessible and advancing the translational paradigm of TE from research to a competitive commercial field. [61]