Related Research Articles
Azotemia is a medical condition characterized by abnormally high levels of nitrogen-containing compounds in the blood. It is largely related to insufficient or dysfunctional filtering of blood by the kidneys. It can lead to uremia and acute kidney injury if not controlled.

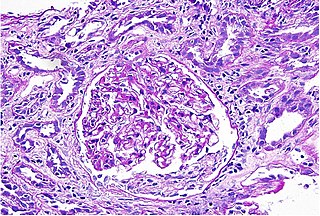
The nephron is the minute or microscopic structural and functional unit of the kidney. It is composed of a renal corpuscle and a renal tubule. The renal corpuscle consists of a tuft of capillaries called a glomerulus and a cup-shaped structure called Bowman's capsule. The renal tubule extends from the capsule. The capsule and tubule are connected and are composed of epithelial cells with a lumen. A healthy adult has 1 to 1.5 million nephrons in each kidney. Blood is filtered as it passes through three layers: the endothelial cells of the capillary wall, its basement membrane, and between the foot processes of the podocytes of the lining of the capsule. The tubule has adjacent peritubular capillaries that run between the descending and ascending portions of the tubule. As the fluid from the capsule flows down into the tubule, it is processed by the epithelial cells lining the tubule: water is reabsorbed and substances are exchanged ; first with the interstitial fluid outside the tubules, and then into the plasma in the adjacent peritubular capillaries through the endothelial cells lining that capillary. This process regulates the volume of body fluid as well as levels of many body substances. At the end of the tubule, the remaining fluid—urine—exits: it is composed of water, metabolic waste, and toxins.

Renal physiology is the study of the physiology of the kidney. This encompasses all functions of the kidney, including maintenance of acid-base balance; regulation of fluid balance; regulation of sodium, potassium, and other electrolytes; clearance of toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.

The proximal tubule is the segment of the nephron in kidneys which begins from the renal pole of the Bowman's capsule to the beginning of loop of Henle. At this location, the glomerular parietal epithelial cells (PECs) lining bowman’s capsule abruptly transition to proximal tubule epithelial cells (PTECs). The proximal tubule can be further classified into the proximal convoluted tubule (PCT) and the proximal straight tubule (PST).

Acute kidney injury (AKI), previously called acute renal failure (ARF), is a sudden decrease in kidney function that develops within 7 days, as shown by an increase in serum creatinine or a decrease in urine output, or both.
Nephrotoxicity is toxicity in the kidneys. It is a poisonous effect of some substances, both toxic chemicals and medications, on kidney function. There are various forms, and some drugs may affect kidney function in more than one way. Nephrotoxins are substances displaying nephrotoxicity.

Renal tubular acidosis (RTA) is a medical condition that involves an accumulation of acid in the body due to a failure of the kidneys to appropriately acidify the urine. In renal physiology, when blood is filtered by the kidney, the filtrate passes through the tubules of the nephron, allowing for exchange of salts, acid equivalents, and other solutes before it drains into the bladder as urine. The metabolic acidosis that results from RTA may be caused either by insufficient secretion of hydrogen ions into the latter portions of the nephron or by failure to reabsorb sufficient bicarbonate ions from the filtrate in the early portion of the nephron. Although a metabolic acidosis also occurs in those with chronic kidney disease, the term RTA is reserved for individuals with poor urinary acidification in otherwise well-functioning kidneys. Several different types of RTA exist, which all have different syndromes and different causes. RTA is usually an incidental finding based on routine blood draws that show abnormal results. Clinically, patients may present with vague symptoms such as dehydration, mental status changes, or delayed growth in adolescents.
Urinary casts are microscopic cylindrical structures produced by the kidney and present in the urine in certain disease states. They form in the distal convoluted tubule and collecting ducts of nephrons, then dislodge and pass into the urine, where they can be detected by microscopy.
Interstitial nephritis, also known as tubulointerstitial nephritis, is inflammation of the area of the kidney known as the renal interstitium, which consists of a collection of cells, extracellular matrix, and fluid surrounding the renal tubules. It is also known as intestinal nephritis because the clinical picture may include mesenteric lymphadenitis in some cases of acute pyelonephritis. More specifically, in case of recurrent urinary tract infection, secondary infection can spread to adjacent intestine. In addition to providing a scaffolding support for the tubular architecture, the interstitium has been shown to participate in the fluid and electrolyte exchange as well as endocrine functions of the kidney.
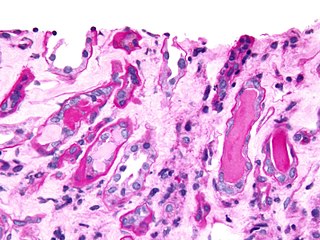
Phosphate nephropathy or nephrocalcinosis is an adverse renal condition that arises with a formation of phosphate crystals within the kidney's tubules. This renal insufficiency is associated with the use of oral sodium phosphate (OSP) such as C.B. Fleet's Phospho soda and Salix's Visocol, for bowel cleansing prior to a colonoscopy.
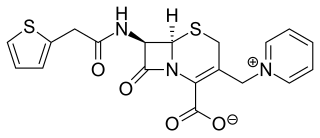
Cephaloridine is a first-generation semisynthetic derivative of antibiotic cephalosporin C. It is a Beta lactam antibiotic, like penicillin. Its chemical structure contains 3 cephems, 4 carboxyl groups and three pyridinium methyl groups.

Low density lipoprotein receptor-related protein 2 also known as LRP-2 or megalin is a protein which in humans is encoded by the LRP2 gene.
Sickle cell nephropathy is a type of nephropathy associated with sickle cell disease which causes kidney complications as a result of sickling of red blood cells in the small blood vessels. The hypertonic and relatively hypoxic environment of the renal medulla, coupled with the slow blood flow in the vasa recta, favors sickling of red blood cells, with resultant local infarction. Functional tubule defects in patients with sickle cell disease are likely the result of partial ischemic injury to the renal tubules.
Renal stem cells are self-renewing, multipotent stem cells which are able to give rise to all the cell types of the kidney. It is involved in the homeostasis and repair of the kidney, and holds therapeutic potential for treatment of kidney failure.

The organic anion transporter 1 (OAT1) also known as solute carrier family 22 member 6 (SLC22A6) is a protein that in humans is encoded by the SLC22A6 gene. It is a member of the organic anion transporter (OAT) family of proteins. OAT1 is a transmembrane protein that is expressed in the brain, the placenta, the eyes, smooth muscles, and the basolateral membrane of proximal tubular cells of the kidneys. It plays a central role in renal organic anion transport. Along with OAT3, OAT1 mediates the uptake of a wide range of relatively small and hydrophilic organic anions from plasma into the cytoplasm of the proximal tubular cells of the kidneys. From there, these substrates are transported into the lumen of the nephrons of the kidneys for excretion. OAT1 homologs have been identified in rats, mice, rabbits, pigs, flounders, and nematodes.
Fanconi syndrome or Fanconi's syndrome is a syndrome of inadequate reabsorption in the proximal renal tubules of the kidney. The syndrome can be caused by various underlying congenital or acquired diseases, by toxicity, or by adverse drug reactions. It results in various small molecules of metabolism being passed into the urine instead of being reabsorbed from the tubular fluid. Fanconi syndrome affects the proximal tubules, namely, the proximal convoluted tubule (PCT), which is the first part of the tubule to process fluid after it is filtered through the glomerulus, and the proximal straight tubule, which leads to the descending limb of loop of Henle.
Renal cortical necrosis (RCN) is a rare cause of acute kidney failure. The condition is "usually caused by significantly diminished arterial perfusion of the kidneys due to spasms of the feeding arteries, microvascular injury, or disseminated intravascular coagulation" and is the pathological progression of acute tubular necrosis. It is frequently associated with obstetric catastrophes such as abruptio placentae and septic shock, and is three times more common in developing nations versus industrialized nations.

Kim Solez is an American pathologist and co-founder of the Banff Classification, the first standardized international classification for renal allograft biopsies. He is also the founder of the Banff Foundation for Allograft Pathology.
Kidney ischemia is a disease with a high morbidity and mortality rate. Blood vessels shrink and undergo apoptosis which results in poor blood flow in the kidneys. More complications happen when failure of the kidney functions result in toxicity in various parts of the body which may cause septic shock, hypovolemia, and a need for surgery. What causes kidney ischemia is not entirely known, but several pathophysiology relating to this disease have been elucidated. Possible causes of kidney ischemia include the activation of IL-17C and hypoxia due to surgery or transplant. Several signs and symptoms include injury to the microvascular endothelium, apoptosis of kidney cells due to overstress in the endoplasmic reticulum, dysfunctions of the mitochondria, autophagy, inflammation of the kidneys, and maladaptive repair.

The mammalian kidneys are a pair of excretory organs of the urinary system of mammals, a type of metanephric kidney. The kidneys in mammals are usually bean-shaped, located behind the peritoneum (retroperitoneally) on the back (dorsal) wall of the body. Each kidney consists of a renal capsule, peripheral cortex, internal medulla, calices, and renal pelvis, although the calices or renal pelvis may be absent in some species. Urine is excreted from the kidney through the ureter. The structure of the kidney may differ between species depending on the environment, in particular on its aridity. The cortex is responsible for filtering the blood, this part of the kidney is similar to the typical kidneys of less developed vertebrates. Nitrogen-containing waste products are excreted by the kidneys in mammals mainly in the form of urea.
References
- ↑ Desanti De Oliveira, B., Xu, K., Shen, T.H. et al. Molecular nephrology: types of acute tubular injury. Nat Rev Nephrol 15, 599–612 (2019). https://doi.org/10.1038/s41581-019-0184-x
- 1 2 3 4 "Acute Tubular Necrosis (ATN)". Nephrology Channel. HealthCommunities.com. 2008. Retrieved 2008-09-23.
- 1 2 Goldman, Lee; Cecil, Russell L. (2008). Cecil medicine. Philadelphia, PA: Saunders Elsevier. p. 705. ISBN 978-0-8089-2377-0. OCLC 191854838.
- ↑ Goldman, Lee; Cecil, Russell L. (2008). Cecil medicine. Philadelphia, PA: Saunders Elsevier. ISBN 978-0-8089-2377-0. OCLC 191854838.[ page needed ]
- ↑ TheFreeDictionary > tubulorrhexis Citing: The American Heritage Medical Dictionary 2007
- ↑ Glynne PA, Picot J, Evans TJ (November 2001). "Coexpressed nitric oxide synthase and apical beta(1) integrins influence tubule cell adhesion after cytokine-induced injury". Journal of the American Society of Nephrology. 12 (11): 2370–83. doi: 10.1681/ASN.V12112370 . PMID 11675413.
- ↑ Glynne PA, Evans TJ (June 1999). "Inflammatory cytokines induce apoptotic and necrotic cell shedding from human proximal tubular epithelial cell monolayers". Kidney International. 55 (6): 2573–97. doi: 10.1046/j.1523-1755.2002.t01-1-00456.x . PMID 10354308.
- ↑ Racusen LC (1998). "Epithelial cell shedding in acute renal injury". Clinical and Experimental Pharmacology & Physiology. 25 (3–4): 273–5. doi:10.1111/j.1440-1681.1998.t01-3-.x. PMID 9590582. S2CID 39727538.
- ↑ Solez K, Racusen LC, Marcussen N, et al. (May 1993). "Morphology of ischemic acute kidney injury, normal function, and cyclosporine toxicity in cyclosporine-treated renal allograft recipients". Kidney International. 43 (5): 1058–67. doi: 10.1038/ki.1993.148 . PMID 8510383.
- ↑ Racusen LC, Fivush BA, Li YL, Slatnik I, Solez K (April 1991). "Dissociation of tubular cell detachment and tubular cell death in clinical and experimental 'acute tubular necrosis'". Laboratory Investigation. 64 (4): 546–56. PMID 1673163.
- ↑ Tulkens, P.M. (March 1989). "Nephrotoxicity of aminoglycoside antibiotics". Toxicology Letters. 46 (1–3): 107–123. doi:10.1016/0378-4274(89)90121-5. PMID 2650018.
- ↑ Banerjee, Debasish; Asif, Arif (May 2003). "Short-Term, High-Dose Pamidronate-Induced Acute Tubular Necrosis: The Postulated Mechanisms of Bisphosphonate Nephrotoxicity". American Journal of Kidney Diseases. 41 (5): e18.1–e18.6. doi:10.1016/S0272-6386(03)00214-2. PMID 12778436.