In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

In human anatomy, a hamstring is any one of the three posterior thigh muscles between the hip and the knee.

The tibia, also known as the shinbone or shankbone, is the larger, stronger, and anterior (frontal) of the two bones in the leg below the knee in vertebrates ; it connects the knee with the ankle. The tibia is found on the medial side of the leg next to the fibula and closer to the median plane. The tibia is connected to the fibula by the interosseous membrane of leg, forming a type of fibrous joint called a syndesmosis with very little movement. The tibia is named for the flute tibia. It is the second largest bone in the human body, after the femur. The leg bones are the strongest long bones as they support the rest of the body.

The posterior cruciate ligament (PCL) is a ligament in each knee of humans and various other animals. It works as a counterpart to the anterior cruciate ligament (ACL). It connects the posterior intercondylar area of the tibia to the medial condyle of the femur. This configuration allows the PCL to resist forces pushing the tibia posteriorly relative to the femur.

The Segond fracture is a type of avulsion fracture from the lateral tibial plateau of the knee, immediately below the articular surface of the tibia.
The drawer test is used in the initial clinical assessment of suspected rupture of the cruciate ligaments in the knee.

Anterior cruciate ligament reconstruction is a surgical tissue graft replacement of the anterior cruciate ligament, located in the knee, to restore its function after an injury. The torn ligament can either be removed from the knee, or preserved before reconstruction through an arthroscopic procedure. ACL repair is also a surgical option. This involves repairing the ACL by re-attaching it, instead of performing a reconstruction. Theoretical advantages of repair include faster recovery and a lack of donor site morbidity, but randomised controlled trials and long-term data regarding re-rupture rates using contemporary surgical techniques are lacking.

The semitendinosus is a long superficial muscle in the back of the thigh. It is so named because it has a very long tendon of insertion. It lies posteromedially in the thigh, superficial to the semimembranosus.

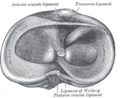
The medial meniscus is a fibrocartilage semicircular band that spans the knee joint medially, located between the medial condyle of the femur and the medial condyle of the tibia. It is also referred to as the internal semilunar fibrocartilage. The medial meniscus has more of a crescent shape while the lateral meniscus is more circular. The anterior aspects of both menisci are connected by the transverse ligament. It is a common site of injury, especially if the knee is twisted.

Cruciate ligaments are pairs of ligaments arranged like a letter X. They occur in several joints of the body, such as the knee joint, wrist joint and the atlanto-axial joint. In a fashion similar to the cords in a toy Jacob's ladder, the crossed ligaments stabilize the joint while allowing a very large range of motion.

An anterior cruciate ligament injury occurs when the anterior cruciate ligament (ACL) is either stretched, partially torn, or completely torn. The most common injury is a complete tear. Symptoms include pain, an audible cracking sound during injury, instability of the knee, and joint swelling. Swelling generally appears within a couple of hours. In approximately 50% of cases, other structures of the knee such as surrounding ligaments, cartilage, or meniscus are damaged.

The patellar tendon is the distal portion of the common tendon of the quadriceps femoris, which is continued from the patella to the tibial tuberosity. It is also sometimes called the patellar ligament as it forms a bone to bone connection when the patella is fully ossified.

The unhappy triad, also known as a blown knee among other names, is an injury to the anterior cruciate ligament, medial collateral ligament, and meniscus. Analysis during the 1990s indicated that this 'classic' O'Donoghue triad is actually an unusual clinical entity among athletes with knee injuries. Some authors mistakenly believe that in this type of injury, "combined anterior cruciate and medial collateral ligament disruptions that were incurred during athletic endeavors" always present with concomitant medial meniscus injury. However, the 1990 analysis showed that lateral meniscus tears are more common than medial meniscus tears in conjunction with sprains of the ACL.

A tear of a meniscus is a rupturing of one or more of the fibrocartilage strips in the knee called menisci. When doctors and patients refer to "torn cartilage" in the knee, they actually may be referring to an injury to a meniscus at the top of one of the tibiae. Menisci can be torn during innocuous activities such as walking or squatting. They can also be torn by traumatic force encountered in sports or other forms of physical exertion. The traumatic action is most often a twisting movement at the knee while the leg is bent. In older adults, the meniscus can be damaged following prolonged 'wear and tear'. Especially acute injuries can lead to displaced tears which can cause mechanical symptoms such as clicking, catching, or locking during motion of the joint. The joint will be in pain when in use, but when there is no load, the pain goes away.
The medial patellofemoral ligament (MPFL) is one of several ligaments on the medial aspect of the knee. It originates in the superomedial aspect of the patella and inserts in the space between the adductor tubercle and the medial femoral epicondyle. The ligament itself extends from the femur to the superomedial patella, and its shape is similar to a trapezoid. It keeps the patella in place, but its main function is to prevent lateral displacement of the patella.
Posterolateral corner injuries of the knee are injuries to a complex area formed by the interaction of multiple structures. Injuries to the posterolateral corner can be debilitating to the person and require recognition and treatment to avoid long term consequences. Injuries to the PLC often occur in combination with other ligamentous injuries to the knee; most commonly the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). As with any injury, an understanding of the anatomy and functional interactions of the posterolateral corner is important to diagnosing and treating the injury.

Medial knee injuries are the most common type of knee injury. The medial ligament complex of the knee consists of:
High tibial osteotomy is an orthopaedic surgical procedure which aims to correct a varus deformation with compartmental osteoarthritis. Since the inception of the procedure, advancements to technique, fixation devices, and a better understanding of patient selection has allowed HTO to become more popular in younger, more active patients hoping to combat arthritis. The idea behind the procedure is to realign the weight-bearing line of the knee. By realigning the knee, the force produced from weight-bearing is shifted from the arthritic, medial compartment to the healthy, lateral compartment. This decrease in force or load in the diseased part of the knee joint decreases knee pain and can delay the development or progression of osteoarthritis in the medial compartment.

The function of the posterior cruciate ligament (PCL) is to prevent the femur from sliding off the anterior edge of the tibia and to prevent the tibia from displacing posterior to the femur. Common causes of PCL injuries are direct blows to the flexed knee, such as the knee hitting the dashboard in a car accident or falling hard on the knee, both instances displacing the tibia posterior to the femur.
Artificial ligaments are devices used to replace damaged ligaments. Today, the most common use of artificial ligaments is in anterior cruciate ligament reconstruction. Although autotransplantation remains the most common method of ligament reconstruction, numerous materials and structures were developed to optimize the artificial ligament since its creation in the World War I era. Many modern artificial ligaments are made of synthetic polymers, such as polyethylene terephthalate. Various coatings have been added to improve the biocompatibility of the synthetic polymers. Early artificial ligaments developed in the 1980s were ineffective due to material deterioration. Currently, the Ligament Advanced Reinforcement System (LARS) artificial ligament has been utilized extensively in clinical applications. Tissue engineering is a growing area of research which aims to regenerate and restore ligament function.