Related Research Articles
Applied ethics is the practical aspect of moral considerations. It is ethics with respect to real-world actions and their moral considerations in private and public life, the professions, health, technology, law, and leadership. For example, bioethics is concerned with identifying the best approach to moral issues in the life sciences, such as euthanasia, the allocation of scarce health resources, or the use of human embryos in research. Environmental ethics is concerned with ecological issues such as the responsibility of government and corporations to clean up pollution. Business ethics includes the duties of whistleblowers to the public and to their employers.
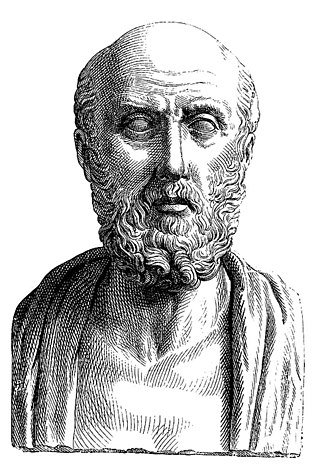
The Hippocratic Oath is an oath of ethics historically taken by physicians. It is one of the most widely known of Greek medical texts. In its original form, it requires a new physician to swear, by a number of healing gods, to uphold specific ethical standards. The oath is the earliest expression of medical ethics in the Western world, establishing several principles of medical ethics which remain of paramount significance today. These include the principles of medical confidentiality and non-maleficence. As the seminal articulation of certain principles that continue to guide and inform medical practice, the ancient text is of more than historic and symbolic value. It is enshrined in the legal statutes of various jurisdictions, such that violations of the oath may carry criminal or other liability beyond the oath's symbolic nature.

Informed consent is a principle in medical ethics, medical law and media studies, that a patient must have sufficient information and understanding before making decisions about their medical care. Pertinent information may include risks and benefits of treatments, alternative treatments, the patient's role in treatment, and their right to refuse treatment. In most systems, healthcare providers have a legal and ethical responsibility to ensure that a patient's consent is informed. This principle applies more broadly than healthcare intervention, for example to conduct research and to disclose a person's medical information.
In developmental psychology and moral, political, and bioethical philosophy, autonomy is the capacity to make an informed, uncoerced decision. Autonomous organizations or institutions are independent or self-governing. Autonomy can also be defined from a human resources perspective, where it denotes a level of discretion granted to an employee in his or her work. In such cases, autonomy is known to generally increase job satisfaction. Self-actualized individuals are thought to operate autonomously of external expectations. In a medical context, respect for a patient's personal autonomy is considered one of many fundamental ethical principles in medicine.
Bioethics is both a field of study and professional practice, interested in ethical issues related to health, including those emerging from advances in biology, medicine, and technologies. It proposes the discussion about moral discernment in society and it is often related to medical policy and practice, but also to broader questions as environment, well-being and public health. Bioethics is concerned with the ethical questions that arise in the relationships among life sciences, biotechnology, medicine, politics, law, theology and philosophy. It includes the study of values relating to primary care, other branches of medicine, ethical education in science, animal, and environmental ethics, and public health.
Medical ethics is an applied branch of ethics which analyzes the practice of clinical medicine and related scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. These values include the respect for autonomy, non-maleficence, beneficence, and justice. Such tenets may allow doctors, care providers, and families to create a treatment plan and work towards the same common goal. It is important to note that these four values are not ranked in order of importance or relevance and that they all encompass values pertaining to medical ethics. However, a conflict may arise leading to the need for hierarchy in an ethical system, such that some moral elements overrule others with the purpose of applying the best moral judgement to a difficult medical situation. Medical ethics is particularly relevant in decisions regarding involuntary treatment and involuntary commitment.
Utilitarian bioethics refers to the branch of bioethics that incorporates principles of utilitarianism to directing practices and resources where they will have the most usefulness and highest likelihood to produce happiness, in regards to medicine, health, and medical or biological research.
Primum non nocere is a Latin phrase that means "first, do no harm". The phrase is sometimes recorded as primum nil nocere.

Human subject research is systematic, scientific investigation that can be either interventional or observational and involves human beings as research subjects, commonly known as test subjects. Human subject research can be either medical (clinical) research or non-medical research. Systematic investigation incorporates both the collection and analysis of data in order to answer a specific question. Medical human subject research often involves analysis of biological specimens, epidemiological and behavioral studies and medical chart review studies. On the other hand, human subject research in the social sciences often involves surveys which consist of questions to a particular group of people. Survey methodology includes questionnaires, interviews, and focus groups.
Harm is a moral and legal concept with multiple definitions. It generally functions as a synonym for evil or anything that is bad under certain moral systems. Something that causes harm is harmful, and something that does not is harmless.
An institutional review board (IRB), also known as an independent ethics committee (IEC), ethical review board (ERB), or research ethics board (REB), is a committee at an institution that applies research ethics by reviewing the methods proposed for research involving human subjects, to ensure that the projects are ethical. The main goal of IRB reviews is to ensure that study participants are not harmed. Such boards are formally designated to approve, monitor, and review biomedical and behavioral research involving humans, and they are legally required in some countries under certain specified circumstances. Most countries use some form of IRB to safeguard ethical conduct of research so that it complies with national and international norms, regulations or codes.
Nursing ethics is a branch of applied ethics that concerns itself with activities in the field of nursing. Nursing ethics shares many principles with medical ethics, such as beneficence, non-maleficence and respect for autonomy. It can be distinguished by its emphasis on relationships, human dignity and collaborative care.
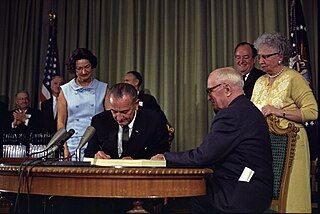
The Belmont Report is a 1978 report created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. Its full title is the Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research, Report of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research.
Research ethics is a discipline within the study of applied ethics. Its scope ranges from general scientific integrity and misconduct to the treatment of human and animal subjects. The societal responsibilities science and reseach has are not traditionally included and less well defined.

Kantian ethics refers to a deontological ethical theory developed by German philosopher Immanuel Kant that is based on the notion that "I ought never to act except in such a way that I could also will that my maxim should become a universal law.” It is also associated with the idea that “[i]t is impossible to think of anything at all in the world, or indeed even beyond it, that could be considered good without limitation except a good will." The theory was developed in the context of Enlightenment rationalism. It states that an action can only be moral if it is motivated by a sense of duty, and its maxim may be rationally willed a universal, objective law.
The philosophy of healthcare is the study of the ethics, processes, and people which constitute the maintenance of health for human beings. For the most part, however, the philosophy of healthcare is best approached as an indelible component of human social structures. That is, the societal institution of healthcare can be seen as a necessary phenomenon of human civilization whereby an individual continually seeks to improve, mend, and alter the overall nature and quality of their life. This perennial concern is especially prominent in modern political liberalism, wherein health has been understood as the foundational good necessary for public life.
Principlism is an applied ethics approach to the examination of moral dilemmas centering the application of certain ethical principles. This approach to ethical decision-making has been prevalently adopted in various professional fields, largely because it sidesteps complex debates in moral philosophy at the theoretical level.
Various organizations have created guidelines for human subject research for various kinds of research involving human subjects and for various situations.
The American Psychological Association (APA) Ethical Principles of Psychologists and Code of Conduct includes an introduction, preamble, a list of five aspirational principles and a list of ten enforceable standards that psychologists use to guide ethical decisions in practice, research, and education. The principles and standards are written, revised, and enforced by the APA. The code of conduct is applicable to psychologists in a variety of areas across a variety of contexts. In the event of a violation of the code of conduct, the APA may take action ranging from termination of the APA membership to the loss of licensure, depending on the violation. Other professional organizations and licensing boards may adopt and enforce the code.
Maternal-fetal conflict, also known as obstetric conflict, occurs when a pregnant individual's (maternal) interests conflict with the interests of the fetus. Legal and ethical considerations involving women's rights and the rights of the fetus as a patient and future child, have become more complicated with advances in medicine and technology. Maternal-fetal conflict can occur in situations where the mother denies health recommendations that can benefit the fetus or make life choices that can harm the fetus. There are maternal-fetal conflict situations where the law becomes involved, but most physicians avoid involving the law for various reasons.
References
- ↑ "6.4.2 Beneficence". www.bitbybitbook.com. Retrieved 2021-04-24.
- ↑ Ross, W.D. (1988). The Right and the Good. Indianapolis: Hackett Pub. Co. p. 21. ISBN 978-0-87220-058-6.
- ↑ Levine, Robert J. (1988). Ethics and Regulation of Clinical Research (2nd ed.). New Haven, CT: Yale University Press. ISBN 978-0-300-04288-7.
- ↑ Graff, James A. (1963). "Human Acts, an Essay in their Moral Evaluation by Eric D'Arcy, The Clarendon Press, Oxford, 1963, 174p. $4.50". Dialogue. 3 (3): 311–2. doi:10.1017/S0012217300035460. S2CID 170741246.
- ↑ Young, Michael; Wagner, Angela (2023), "Medical Ethics", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30570982 , retrieved 2023-11-24
- ↑ King, Ruth R.; Faden, Tom L. Beauchamp (1986). A History and Theory of Informed Consent. In collaboration with Nancy, M.P. ([Online-Ausg.]. ed.). New York: Oxford University Press. pp. 11. ISBN 0-19-503686-7.