Gestation is the period of development during the carrying of an embryo, and later fetus, inside viviparous animals. It is typical for mammals, but also occurs for some non-mammals. Mammals during pregnancy can have one or more gestations at the same time, for example in a multiple birth.
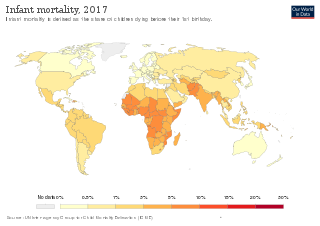
Infant mortality is the death of an infant before the infant's first birthday. The occurrence of infant mortality in a population can be described by the infant mortality rate (IMR), which is the number of deaths of infants under one year of age per 1,000 live births. Similarly, the child mortality rate, also known as the under-five mortality rate, compares the death rate of children up to the age of five.

Maternal death or maternal mortality is defined in slightly different ways by several different health organizations. The World Health Organization (WHO) defines maternal death as the death of a pregnant mother due to complications related to pregnancy, underlying conditions worsened by the pregnancy or management of these conditions. This can occur either while she is pregnant or within six weeks of resolution of the pregnancy. The CDC definition of pregnancy-related deaths extends the period of consideration to include one year from the resolution of the pregnancy. Pregnancy associated death, as defined by the American College of Obstetricians and Gynecologists (ACOG), are all deaths occurring within one year of a pregnancy resolution. Identification of pregnancy associated deaths is important for deciding whether or not the pregnancy was a direct or indirect contributing cause of the death.
Health equity arises from access to the social determinants of health, specifically from wealth, power and prestige. Individuals who have consistently been deprived of these three determinants are significantly disadvantaged from health inequities, and face worse health outcomes than those who are able to access certain resources. It is not equity to simply provide every individual with the same resources; that would be equality. In order to achieve health equity, resources must be allocated based on an individual need-based principle.
Maternal health is the health of women during pregnancy, childbirth, and the postpartum period. In most cases, maternal health encompasses the health care dimensions of family planning, preconception, prenatal, and postnatal care in order to ensure a positive and fulfilling experience. In other cases, maternal health can reduce maternal morbidity and mortality. Maternal health revolves around the health and wellness of pregnant women, particularly when they are pregnant, at the time they give birth, and during child-raising. WHO has indicated that even though motherhood has been considered as a fulfilling natural experience that is emotional to the mother, a high percentage of women develop health problems and sometimes even die. Because of this, there is a need to invest in the health of women. The investment can be achieved in different ways, among the main ones being subsidizing the healthcare cost, education on maternal health, encouraging effective family planning, and ensuring progressive check up on the health of women with children. Maternal morbidity and mortality particularly affects women of color and women living in low and lower-middle income countries.

Reproductive justice is a critical feminist framework that was invented as a response to United States reproductive politics. The three core values of reproductive justice are the right to have a child, the right to not have a child, and the right to parent a child or children in safe and healthy environments. The framework moves women's reproductive rights past a legal and political debate to incorporate the economic, social, and health factors that impact women's reproductive choices and decision-making ability.
Unintended pregnancies are pregnancies that are mistimed, unplanned or unwanted at the time of conception.
Black Women's Health Imperative, previously the National Black Women's Health Project, was formed in 1983 in Atlanta, Georgia out of a need to address the health and reproductive rights of African American women. NBWHP was principally founded by Byllye Avery. Avery was involved in reproductive healthcare work in Gainesville, Florida in the 1970s and was particularly influenced by the impact that policy had on women of color and poor women. Additionally Avery was also concerned with healthcare choices and wanted "to provide an environment where women could feel comfortable and take control of their own health".
Research shows many health disparities among different racial and ethnic groups in the United States. Different outcomes in mental and physical health exist between all U.S. Census-recognized racial groups, but these differences stem from different historical and current factors, including genetics, socioeconomic factors, and racism. Research has demonstrated that numerous health care professionals show implicit bias in the way that they treat patients. Certain diseases have a higher prevalence among specific racial groups, and life expectancy also varies across groups.
Prenatal care in the United States is a health care preventive care protocol recommended to women with the goal to provide regular check-ups that allow obstetricians-gynecologists, family medicine physicians, or midwives to detect, treat and prevent potential health problems throughout the course of pregnancy while promoting healthy lifestyles that benefit both mother and child. Patients are encouraged to attend monthly checkups during the first two trimesters and in the third trimester gradually increasing to weekly visits. Women who suspect they are pregnant can schedule pregnancy tests prior to 9 weeks gestation. Once pregnancy is confirmed an initial appointment is scheduled after 8 weeks gestation. Subsequent appointments consist of various tests ranging from blood pressure to glucose levels to check on the health of the mother and fetus. If not, appropriate treatment will then be provided to hinder any further complications.
This article summarizes healthcare in Texas. In 2022, the United Healthcare Foundation ranked Texas as the 38th healthiest state in the United States. Obesity, excessive drinking, maternal mortality, infant mortality, vaccinations, mental health, and limited access to healthcare are among the major public health issues facing Texas.
Women's reproductive health in the United States refers to the set of physical, mental, and social issues related to the health of women in the United States. It includes the rights of women in the United States to adequate sexual health, available contraception methods, and treatment for sexually transmitted diseases. The prevalence of women's health issues in American culture is inspired by second-wave feminism in the United States. As a result of this movement, women of the United States began to question the largely male-dominated health care system and demanded a right to information on issues regarding their physiology and anatomy. The U.S. government has made significant strides to propose solutions, like creating the Women's Health Initiative through the Office of Research on Women's Health in 1991. However, many issues still exist related to the accessibility of reproductive healthcare as well as the stigma and controversy attached to sexual health, contraception, and sexually transmitted diseases.

Maternal healthcare in Texas refers to the provision of family planning services, abortion options, pregnancy-related services, and physical and mental well-being care for women during the prenatal and postpartum periods. The provision of maternal health services in each state can prevent and reduce the incidence of maternal morbidity and mortality and fetal death.

Maternal mortality refers to the death of a woman during her pregnancy or up to a year after her pregnancy has terminated; this metric only includes causes related to the pregnancy, and does not include accidental causes. Some sources will define maternal mortality as the death of a woman up to 42 days after the pregnancy has ended, instead of one year. In 1986, the CDC began tracking pregnancy-related deaths to gather information and determine what was causing these deaths by creating the Pregnancy-Related Mortality Surveillance System. According to a 2010-2011 report although the United States was spending more on healthcare than any other country in the world, more than two women died during childbirth every day, making maternal mortality in the United States the highest when compared to 49 other countries in the developed world.
The weathering hypothesis was proposed to account for early health deterioration as a result of cumulative exposure to experiences of social, economic, and political adversity. It is well documented that minority groups and marginalized communities suffer from poorer health outcomes. This may be due to a multitude of stressors including prejudice, social alienation, institutional bias, political oppression, economic exclusion, and racial discrimination. The weathering hypothesis proposes that the cumulative burden of these stressors as individuals age is "weathering", and the increased weathering experienced by minority groups compared to others can account for differences in health outcomes. In recent years, the biological plausibility of the weathering hypothesis has been investigated in studies evaluating the physiological effects of social, environmental and political stressors among marginalized communities. This has led to more widespread use of the weathering hypothesis as a framework for explaining health disparities on the basis of differential exposure to racially based stressors. Researchers have also identified patterns connecting weathering to biological phenomena associated with stress and aging, such as allostatic load, epigenetics, telomere shortening, and accelerated brain aging.

The COVID-19 pandemic has revealed race-based health care disparities in many countries, including the United States, United Kingdom, Norway, Sweden, Canada, and Singapore. These disparities are believed to originate from structural racism in these countries which pre-dates the pandemic; a commentary in The BMJ noted that "ethnoracialised differences in health outcomes have become the new normal across the world" as a result of ethnic and racial disparities in COVID-19 healthcare, determined by social factors. Data from the United States and elsewhere shows that minorities, especially black people, have been infected and killed at a disproportionate rate to white people.
Chaniece Wallace, a black woman and physician, died at 30 years of age from complications of pregnancy two days after the birth of her daughter. Her death is seen as preventable and is viewed in the context of high rates of maternal mortality in the United States, particularly among the African American population. It is cited as an example in medical and scholarly publications to call for improved health outcomes in the black U.S. population. Wallace died despite several factors seen as protective: she was "highly educated, employed as a health care practitioner, had access to health care, and had a supportive family." Wallace was a fourth year pediatric chief resident at the Indiana University School of Medicine and was working at Riley Children's Health Hospital at the time of her death.
Maternal health outcomes differ significantly between racial groups within the United States. The American College of Obstetricians and Gynecologists describes these disparities in obstetric outcomes as "prevalent and persistent." Black, indigenous, and people of color are disproportionately affected by many of the maternal health outcomes listed as national objectives in the U.S. Department of Health and Human Services's national health objectives program, Healthy People 2030. The American Public Health Association considers maternal mortality to be a human rights issue, also noting the disparate rates of Black maternal death. Race affects maternal health throughout the pregnancy continuum, beginning prior to conception and continuing through pregnancy (antepartum), during labor and childbirth (intrapartum), and after birth (postpartum).
The COVID-19 pandemic has had an unequal impact on different racial and ethnic groups in the United States, resulting in new disparities of health outcomes as well as exacerbating existing health and economic disparities.

Maternity care deserts in the United States, also known as maternal care deserts, are counties that lack maternity care resources. The March of Dimes defines a maternity care desert as a county that has no hospitals or birth centers offering obstetric care and no obstetric providers. As of 2020 March of Dimes classified 1095 of 3139 of U.S. counties (34.9%) as maternity care deserts. Its 2022 report indicated an increase of nearly 2%, with 1119 of 3142 US counties (35.6%) considered maternity care deserts, affecting a population of over 5.6 million women. People living in maternity care deserts may have to travel longer distances to receive care, which is associated with higher costs and a greater risk of pregnancy complications.