Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

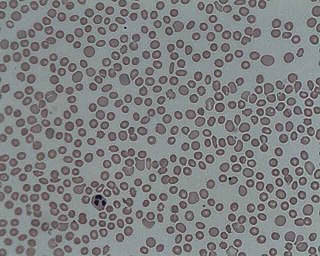
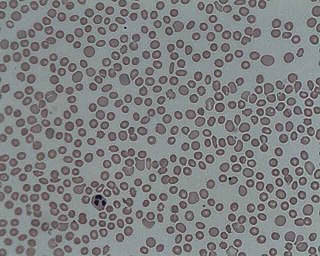
Bone marrow is a semi-solid tissue found within the spongy portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production. It is composed of hematopoietic cells, marrow adipose tissue, and supportive stromal cells. In adult humans, bone marrow is primarily located in the ribs, vertebrae, sternum, and bones of the pelvis. Bone marrow comprises approximately 5% of total body mass in healthy adult humans, such that a man weighing 73 kg (161 lbs) will have around 3.7 kg (8 lbs) of bone marrow.
In hematology, thrombocytopenia is a condition characterized by abnormally low levels of platelets in the blood. Low levels of platelets in turn may lead to prolonged or excessive bleeding. It is the most common coagulation disorder among intensive care patients and is seen in a fifth of medical patients and a third of surgical patients.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Plateletpheresis is the process of collecting thrombocytes, more commonly called platelets, a component of blood involved in blood clotting. The term specifically refers to the method of collecting the platelets, which is performed by a device used in blood donation that separates the platelets and returns other portions of the blood to the donor. Platelet transfusion can be a life-saving procedure in preventing or treating serious complications from bleeding and hemorrhage in patients who have disorders manifesting as thrombocytopenia or platelet dysfunction. This process may also be used therapeutically to treat disorders resulting in extraordinarily high platelet counts such as essential thrombocytosis.
Lymph node biopsy is a test in which a lymph node or a piece of a lymph node is removed for examination under a microscope.

Fine-needle aspiration (FNA) is a diagnostic procedure used to investigate lumps or masses. In this technique, a thin, hollow needle is inserted into the mass for sampling of cells that, after being stained, are examined under a microscope (biopsy). The sampling and biopsy considered together are called fine-needle aspiration biopsy (FNAB) or fine-needle aspiration cytology (FNAC). Fine-needle aspiration biopsies are very safe minor surgical procedures. Often, a major surgical biopsy can be avoided by performing a needle aspiration biopsy instead, eliminating the need for hospitalization. In 1981, the first fine-needle aspiration biopsy in the United States was done at Maimonides Medical Center. Today, this procedure is widely used in the diagnosis of cancer and inflammatory conditions. Fine needle aspiration is generally considered a safe procedure. Complications are infrequent.

The endometrial biopsy is a medical procedure that involves taking a tissue sample of the lining of the uterus. The tissue subsequently undergoes a histologic evaluation which aids the physician in forming a diagnosis.
Arthrocentesis, or joint aspiration, is the clinical procedure performed to diagnose and, in some cases, treat musculoskeletal conditions. The procedure entails using a syringe to collect synovial fluid from or inject medication into the joint capsule. Laboratory analysis of synovial fluid can further help characterize the diseased joint and distinguish between gout, arthritis, and synovial infections such as septic arthritis.

Skin biopsy is a biopsy technique in which a skin lesion is removed to be sent to a pathologist to render a microscopic diagnosis. It is usually done under local anesthetic in a physician's office, and results are often available in 4 to 10 days. It is commonly performed by dermatologists. Skin biopsies are also done by family physicians, internists, surgeons, and other specialties. However, performed incorrectly, and without appropriate clinical information, a pathologist's interpretation of a skin biopsy can be severely limited, and therefore doctors and patients may forgo traditional biopsy techniques and instead choose Mohs surgery.

Basophilia is the condition of having greater than 200 basophils/μL in the venous blood. Basophils are the least numerous of the myelogenous cells, and it is rare for their numbers to be abnormally high without changes to other blood components. Rather, basophilia is most often coupled with other white blood cell conditions such as eosinophilia, high levels of eosinophils in the blood. Basophils are easily identifiable by a blue coloration of the granules within each cell, marking them as granulocytes, in addition to segmented nuclei.
Acute myelomonocytic leukemia (AMML) is a form of acute myeloid leukemia that involves a proliferation of CFU-GM myeloblasts and monoblasts. AMML occurs with a rapid increase amount in white blood cell count and is defined by more than 20% of myeloblast in the bone marrow. It is classified under "M4" in the French-American-British classification (FAB). It is classified under "AML, not otherwise classified" in the WHO classification.

Congenital amegakaryocytic thrombocytopenia (CAMT) is a rare autosomal recessive bone marrow failure syndrome characterized by severe thrombocytopenia, which can progress to aplastic anemia and leukemia. CAMT usually manifests as thrombocytopenia in the initial month of life or in the fetal phase. Typically CAMPT presents with petechiae, cerebral bleeds, recurrent rectal bleeding, or pulmonary hemorrhage.

Renal biopsy is a medical procedure in which a small piece of kidney is removed from the body for examination, usually under a microscope. Microscopic examination of the tissue can provide information needed to diagnose, monitor or treat problems of the kidney.
Gestational (incidental) thrombocytopenia is a condition that commonly affects pregnant women. Thrombocytopenia is defined as the drop in platelet count from the normal range of 150,000–400,000/μL to a count lower than 150,000/μL. There is still ongoing research to determine the reason for the lowering of platelet count in women with a normal pregnancy. Some researchers speculate the cause to be dependent on dilution, decreased production of platelets, or an increased turnover event. Although women with normal pregnancy experience a low platelet count, women experiencing a continuous drop in platelet will be diagnosed with thrombocytopenia and women with levels greater than 70,000/μL will be diagnosed with gestational thrombocytopenia.

The Jamshidi needle is a trephine needle for performing bone marrow biopsy, whereby a cylindrical sample of tissue, a core biopsy specimen, is obtained. It is a cylindrical needle with a tapered cutting tip. The tapered end reduces the potential of crush artifact. It is the most commonly used needle for performing bone marrow biopsies. The device is named for its inventor Khosrow Jamshidi who is an Iranian physician.

A breast biopsy is usually done after a suspicious lesion is discovered on either mammography or ultrasound to get tissue for pathological diagnosis. Several methods for a breast biopsy now exist. The most appropriate method of biopsy for a patient depends upon a variety of factors, including the size, location, appearance and characteristics of the abnormality. The different types of breast biopsies include fine-needle aspiration (FNA), vacuum-assisted biopsy, core needle biopsy, and surgical excision biopsy. Breast biopsies can be done utilizing ultrasound, MRI or a stereotactic biopsy imaging guidance. Vacuum assisted biopsies are typically done using stereotactic techniques when the suspicious lesion can only be seen on mammography. On average, 5–10 biopsies of a suspicious breast lesion will lead to the diagnosis of one case of breast cancer. Needle biopsies have largely replaced open surgical biopsies in the initial assessment of imaging as well as palpable abnormalities in the breast.

In medicine, sampling is gathering of matter from the body to aid in the process of a medical diagnosis and/or evaluation of an indication for treatment, further medical tests or other procedures. In this sense, the sample is the gathered matter, and the sampling tool or sampler is the person or material to collect the sample.
Suprapubic aspiration is a procedure to take a urine sample. It involves putting a needle through the skin just above the pubic bone into the bladder. It is typically used as a method to collect urine in child less than 2 years of age who is not yet toilet trained in an effort to diagnose a urinary tract infection.
A bone biopsy is a procedure in which a small bone sample is removed from the outer layers of bone for examination, unlike a bone marrow biopsy, which involves the innermost part of the bone. The bone biopsy sample retains the architecture of bone when seen using histopathological examination slide.