Community health refers to simple health services that are delivered by laymen outside hospitals and clinics. Community health is also the subset of public health that is taught to and practiced by clinicians as part of their normal duties. Community health volunteers and community health workers work with primary care providers to facilitate entry into, exit from and utilization of the formal health system by community members.

Long-term care (LTC) is a variety of services which help meet both the medical and non-medical needs of people with a chronic illness or disability who cannot care for themselves for long periods. Long-term care is focused on individualized and coordinated services that promote independence, maximize patients' quality of life, and meet patients' needs over a period of time.

NHS Scotland, sometimes styled NHSScotland, is the publicly funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, supported by seven special non-geographic health boards, and Public Health Scotland.
Health and Social Care (HSC) is the publicly funded healthcare system in Northern Ireland. Although having been created separately to the National Health Service (NHS), it is nonetheless considered a part of the overall national health service in the United Kingdom. The Northern Ireland Executive through its Department of Health is responsible for its funding, while the Public Health Agency is the executive agency responsible for the provision of public health and social care services across Northern Ireland. It is free of charge to all citizens of Northern Ireland and the rest of the United Kingdom.

Deinstitutionalisation is the process of replacing long-stay psychiatric hospitals with less isolated community mental health services for those diagnosed with a mental disorder or developmental disability. In the late 20th century, it led to the closure of many psychiatric hospitals, as patients were increasingly cared for at home, in halfway houses and clinics, in regular hospitals, or not at all.
A group home, congregate living facility, care home, adult family home, etc., is a structured and supervised residence model that provides assisted living and medical care for those with complex health needs. Traditionally, the model has been used for children or young people who cannot live with their families or afford their own homes, people with chronic disabilities who may be adults or seniors, or people with dementia and related aged illnesses. Typically, there are no more than six residents, and there is at least one trained caregiver there 24 hours a day. In some early "model programs", a house manager, night manager, weekend activity coordinator, and four part-time skill teachers were reported. Originally, the term group home referred to homes of 8 to 16 individuals, which was a state-mandated size during deinstitutionalization. Residential nursing facilities, also included in this article, may be as large as 100 individuals in 2015, which is no longer the case in fields such as intellectual and developmental disabilities. Depending on the severity of the condition requiring one to need to live in a group home, some clients are able to attend day programs and most clients are able to live normal lifestyles.
The psychiatric survivors movement is a diverse association of individuals who either currently access mental health services, or who have experienced interventions by psychiatry they consider unhelpful, harmful, abusive or illegal.
The Direct Payments scheme is a UK Government initiative in the field of Social Services that gives users money directly to pay for their own care, rather than the traditional route of a Local Government Authority providing care for them. The Cabinet Office Strategy Unit calls direct payments "the most successful public policy in the area of social care".
Community mental health services (CMHS), also known as community mental health teams (CMHT) in the United Kingdom, support or treat people with mental disorders in a domiciliary setting, instead of a psychiatric hospital (asylum). The array of community mental health services vary depending on the country in which the services are provided. It refers to a system of care in which the patient's community, not a specific facility such as a hospital, is the primary provider of care for people with a mental illness. The goal of community mental health services often includes much more than simply providing outpatient psychiatric treatment.
Special needs dentistry, also known as special care dentistry, is a dental specialty that deals with the oral health problems of geriatric patients, patients with intellectual disabilities, and patients with other medical, physical, or psychiatric issues.
In England, social care is defined as the provision of social work, personal care, protection or social support services to children or adults in need or at risk, or adults with needs arising from illness, disability, old age or poverty. The main legal definitions flow from the National Health Service and Community Care Act 1990, with other provisions covering disability and responsibilities to informal carers. That provision may have one or more of the following aims: to protect people who use care services from abuse or neglect, to prevent deterioration of or promote physical or mental health, to promote independence and social inclusion, to improve opportunities and life chances, to strengthen families and to protect human rights in relation to people's social needs.
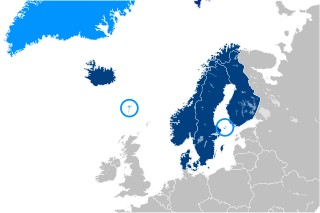
Social security or welfare in Finland is very comprehensive compared to what almost all other countries provide. In the late 1980s, Finland had one of the world's most advanced welfare systems, which guaranteed decent living conditions to all Finns. Created almost entirely during the first three decades after World War II, the social security system was an outgrowth of the traditional Nordic belief that the state is not inherently hostile to the well-being of its citizens and can intervene benevolently on their behalf. According to some social historians, the basis of this belief was a relatively benign history that had allowed the gradual emergence of a free and independent peasantry in the Nordic countries and had curtailed the dominance of the nobility and the subsequent formation of a powerful right wing. Finland's history was harsher than the histories of the other Nordic countries but didn't prevent the country from following their path of social development.

Jack Tizard CBE was a research psychologist, professor of child development, research unit director, international adviser on learning disability and child care, and a president of the British Psychological Society. Tizard was born in New Zealand but spent most of his professional life in England where, as a psychologist, he worked at the boundaries of psychology, medicine, education and the social sciences. His work on alternatives to institutional care in the 1950s and 1960s underpinned the subsequent development of 'ordinary life' models for children and adults with learning disabilities. His later work focused on developing services for young children and their families. Tizard's approach was characterised by a commitment to using high research standards to address important social problems, ensuring through his extensive advisory activities that the results of research were available to practitioners and policy-makers.

In a study in Western societies, homeless people have a higher prevalence of mental illness when compared to the general population. They also are more likely to suffer from alcoholism and drug dependency. It is estimated that 20–25% of homeless people, compared with 6% of the non-homeless, have severe mental illness. Others estimate that up to one-third of the homeless have a mental illness. In January 2015, the most extensive survey ever undertaken found 564,708 people were homeless on a given night in the United States. Depending on the age group in question and how homelessness is defined, the consensus estimate as of 2014 was that, at minimum, 25% of the American homeless—140,000 individuals—were seriously mentally ill at any given point in time. 45% percent of the homeless—250,000 individuals—had any mental illness. More would be labeled homeless if these were annual counts rather than point-in-time counts. Being chronically homeless also means that people with mental illnesses are more likely to experience catastrophic health crises requiring medical intervention or resulting in institutionalization within the criminal justice system. Majority of the homeless population do not have a mental illness. Although there is no correlation between homelessness and mental health, those who are dealing with homelessness are struggling with psychological and emotional distress. The Substance Abuse and Mental Health Services Administration conducted a study and found that in 2010, 26.2 percent of sheltered homeless people had a severe mental illness.
The Banyan is a non-governmental organization based in Chennai, India that was founded in 1993 by Vandana Gopikumar and Vaishnavi Jayakumar to cater to mentally-ill and homeless women in the city.
Mental health in the Philippines is a survey of the status of psychological, psychiatric, and emotional health care in the Philippines from both past and present programs.
As of 2017, approximately 1.4 million Americans live in a nursing home, two-thirds of whom rely on Medicaid to pay for their care. Residential nursing facilities receive Medicaid federal funding and approvals through a state health department. These facilities may be overseen by various types of state agency.
The United States has experienced two waves of deinstitutionalization, the process of replacing long-stay psychiatric hospitals with less isolated community mental health services for those diagnosed with a mental disorder or developmental disability.
Mental health in the United Kingdom involves state, private and community sector intervention in mental health issues. One of the first countries to build asylums, the United Kingdom was also one of the first countries to turn away from them as the primary mode of treatment for the mentally ill. The 1960s onwards saw a shift towards Care in the Community, which is a form of deinstitutionalisation. The majority of mental health care is now provided by the National Health Service (NHS), assisted by the private and the voluntary sectors.