Related Research Articles

Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. These may occur a few times a day or a few times per week. Depending on the person, asthma symptoms may become worse at night or with exercise.

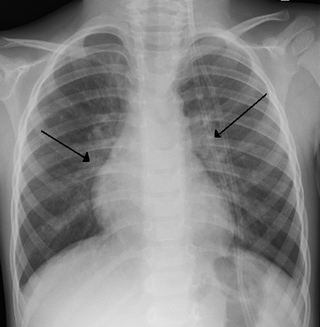
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of the condition is variable.

A cough is a sudden expulsion of air through the large breathing passages which can help clear them of fluids, irritants, foreign particles and microbes. As a protective reflex, coughing can be repetitive with the cough reflex following three phases: an inhalation, a forced exhalation against a closed glottis, and a violent release of air from the lungs following opening of the glottis, usually accompanied by a distinctive sound.

Cold medicines are a group of medications taken individually or in combination as a treatment for the symptoms of the common cold and similar conditions of the upper respiratory tract. The term encompasses a broad array of drugs, including analgesics, antihistamines and decongestants, among many others. It also includes drugs which are marketed as cough suppressants or antitussives, but their effectiveness in reducing cough symptoms is unclear or minimal.
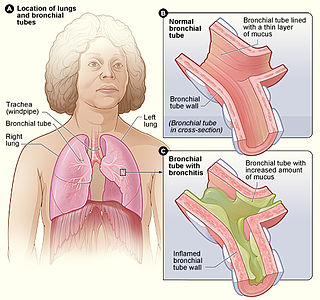
Acute bronchitis, also known as a chest cold, is short-term bronchitis – inflammation of the bronchi of the lungs. The most common symptom is a cough. Other symptoms include coughing up mucus, wheezing, shortness of breath, fever, and chest discomfort. The infection may last from a few to ten days. The cough may persist for several weeks afterward with the total duration of symptoms usually around three weeks. Some have symptoms for up to six weeks.

Bronchiectasis is a disease in which there is permanent enlargement of parts of the airways of the lung. Symptoms typically include a chronic cough with mucus production. Other symptoms include shortness of breath, coughing up blood, and chest pain. Wheezing and nail clubbing may also occur. Those with the disease often get lung infections.
Bronchiolitis is inflammation of the small airways in the lungs. Acute bronchiolitis is due to a viral infection usually affecting children younger than two years of age. Symptoms may include fever, cough, runny nose, wheezing, and breathing problems. More severe cases may be associated with nasal flaring, grunting, or the skin between the ribs pulling in with breathing. If the child has not been able to feed properly, signs of dehydration may be present.

Respiratory syncytial virus (RSV), also called human respiratory syncytial virus (hRSV) and human orthopneumovirus, is a contagious virus that causes infections of the respiratory tract. It is a negative-sense, single-stranded RNA virus. Its name is derived from the large cells known as syncytia that form when infected cells fuse.

Laryngitis is inflammation of the larynx. Symptoms often include a hoarse voice and may include fever, cough, pain in the front of the neck, and trouble swallowing. Typically, these last under two weeks.
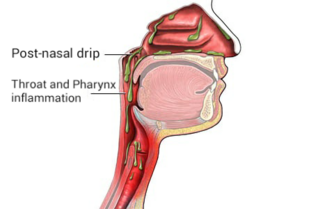
Post-nasal drip (PND), also known as upper airway cough syndrome (UACS), occurs when excessive mucus is produced by the nasal mucosa. The excess mucus accumulates in the back of the nose, and eventually in the throat once it drips down the back of the throat. It can be caused by rhinitis, sinusitis, gastroesophageal reflux disease (GERD), or by a disorder of swallowing. Other causes can be allergy, cold, flu, and side effects from medications.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.
Acute severe asthma, also known as status asthmaticus, is an acute exacerbation of asthma that does not respond to standard treatments of bronchodilators (inhalers) and corticosteroids. Asthma is caused by multiple genes, some having protective effect, with each gene having its own tendency to be influenced by the environment although a genetic link leading to acute severe asthma is still unknown. Symptoms include chest tightness, rapidly progressive dyspnea, dry cough, use of accessory respiratory muscles, fast and/or labored breathing, and extreme wheezing. It is a life-threatening episode of airway obstruction and is considered a medical emergency. Complications include cardiac and/or respiratory arrest. The increasing prevalence of atopy and asthma remains unexplained but may be due to infection with respiratory viruses.
Occupational asthma is new onset asthma or the recurrence of previously quiescent asthma directly caused by exposure to an agent at workplace. It is an occupational lung disease and a type of work-related asthma. Agents that can induce occupational asthma can be grouped into sensitizers and irritants.
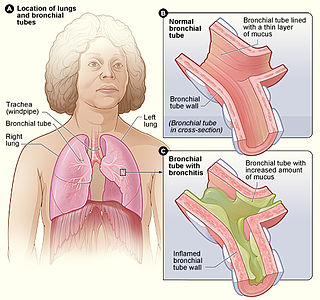
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.
Vocal cord dysfunction (VCD) is a pathology affecting the vocal folds characterized by full or partial vocal fold closure causing difficulty and distress during respiration, especially during inhalation.

In medicine, exhaled nitric oxide (eNO) can be measured in a breath test for asthma and other respiratory conditions characterized by airway inflammation. Nitric oxide (NO) is a gaseous molecule produced by certain cell types in an inflammatory response. The fraction of exhaled NO (FENO) is a promising biomarker for the diagnosis, follow-up and as a guide to therapy in adults and children with asthma. The breath test has recently become available in many well-equipped hospitals in developed countries, although its exact role remains unclear.

Eosinophilic bronchitis (EB) is a type of airway inflammation due to excessive mast cell recruitment and activation in the superficial airways as opposed to the smooth muscles of the airways as seen in asthma. It often results in a chronic cough. Lung function tests are usually normal. Inhaled corticosteroids are often an effective treatment.

Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms due to abnormalities of the airways and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.

Chest pain in children is the pain felt in the chest by infants, children and adolescents. In most cases the pain is not associated with the heart. It is primarily identified by the observance or report of pain by the infant, child or adolescent by reports of distress by parents or caregivers. Chest pain is not uncommon in children. Many children are seen in ambulatory clinics, emergency departments and hospitals and cardiology clinics. Most often there is a benign cause for the pain for most children. Some have conditions that are serious and possibly life-threatening. Chest pain in pediatric patients requires careful physical examination and a detailed history that would indicate the possibility of a serious cause. Studies of pediatric chest pain are sparse. It has been difficult to create evidence-based guidelines for evaluation.
Airway clearance therapy is treatment that uses a number of airway clearance techniques to clear the respiratory airways of mucus and other secretions. Several respiratory diseases cause the normal mucociliary clearance mechanism to become impaired resulting in a build-up of mucus which obstructs breathing, and also affects the cough reflex. Mucus build-up can also cause infection, and inflammation, and repeated infections can result in damage to the airways, and the lung tissue.
References
- 1 2 Chung KF, McGarvey L, Song WJ, Chang AB, Lai K, Canning BJ, et al. (June 2022). "Cough hypersensitivity and chronic cough". Nature Reviews. Disease Primers. 8 (1): 45. doi:10.1038/s41572-022-00370-w. PMC 9244241 . PMID 35773287.
- ↑ Morice AH, Fontana GA, Belvisi MG, Birring SS, Chung KF, Dicpinigaitis PV, et al. (June 2007). "ERS guidelines on the assessment of cough". The European Respiratory Journal. 29 (6): 1256–1276. doi: 10.1183/09031936.00101006 . PMID 17540788. S2CID 17331460.
- ↑ Shim JS, Song WJ, Morice AH (March 2020). "Drug-Induced Cough". Physiological Research. 69 (Suppl 1): S81–S92. doi:10.33549/physiolres.934406. PMC 8604055 . PMID 32228014.
- ↑ Krüger K, Holzinger F, Trauth J, Koch M, Heintze C, Gehrke-Beck S (February 2022). "Chronic Cough". Deutsches Ärzteblatt International. 119 (5): 59–65. doi:10.3238/arztebl.m2021.0396. PMC 9059861 . PMID 34918623.
- ↑ Gibson PG (2019-07-31). "Management of Cough". The Journal of Allergy and Clinical Immunology. In Practice. 7 (6): 1724–1729. doi:10.1016/j.jaip.2019.03.050. PMID 31279460. S2CID 195830273.
- ↑ Song WJ, Chang YS, Faruqi S, Kang MK, Kim JY, Kang MG, et al. (March 2016). "Defining Chronic Cough: A Systematic Review of the Epidemiological Literature". Allergy, Asthma & Immunology Research. 8 (2): 146–155. doi:10.4168/aair.2016.8.2.146. PMC 4713878 . PMID 26739408.
- ↑ Perotin JM, Launois C, Dewolf M, Dumazet A, Dury S, Lebargy F, et al. (2018). "Managing patients with chronic cough: challenges and solutions". Therapeutics and Clinical Risk Management. 14: 1041–1051. doi: 10.2147/TCRM.S136036 . PMC 5995432 . PMID 29922064.
- 1 2 3 Pratter MR (January 2006). "Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines". Chest. 129 (1 Suppl): 63S–71S. doi: 10.1378/chest.129.1_suppl.63s . PMID 16428694.
- ↑ Zhang, Mengru; Morice, Alyn H. (2023-08-29). "Unravelling vagal hypersensitivity in chronic cough: A distinct disease". The Journal of Physiology. doi:10.1113/JP284641. ISSN 0022-3751.
- ↑ Dicpinigaitis, Peter V.; Kantar, Ahmad; Enilari, Oladunni; Paravati, Francesco (2018). "Prevalence of Arnold Nerve Reflex in Adults and Children With Chronic Cough". Chest. 153 (3): 675–679. doi:10.1016/j.chest.2017.11.019. ISSN 1931-3543. PMID 29197546.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Morice AH, Fontana GA, Sovijarvi AR, Pistolesi M, Chung KF, Widdicombe J, et al. (September 2004). "The diagnosis and management of chronic cough". The European Respiratory Journal. 24 (3): 481–492. doi: 10.1183/09031936.04.00027804 . PMID 15358710.
- 1 2 3 Yu L, Xu X, Lv H, Qiu Z (May 2015). "Advances in upper airway cough syndrome". The Kaohsiung Journal of Medical Sciences. 31 (5): 223–228. doi: 10.1016/j.kjms.2015.01.005 . PMID 25910556.
- 1 2 3 4 5 6 Truba O, Dąbrowska M, Grabczak E, Arcimowicz M, Rybka A, Rybka M, Krenke R (2017-09-01). "Upper airway disorders in patients with upper airway cough syndrome". European Respiratory Journal. 50 (suppl 61): PA4043. doi:10.1183/1393003.congress-2017.PA4043. ISSN 0903-1936.
- 1 2 3 4 5 6 7 Herregods TV, Pauwels A, Tack J, Smout AJ, Bredenoord AJ (December 2017). "Reflux-cough syndrome: Assessment of temporal association between reflux episodes and cough bursts". Neurogastroenterology and Motility. 29 (12): e13129. doi:10.1111/nmo.13129. PMID 28612466. S2CID 23985242.
- 1 2 3 4 5 6 Nsouli T, Diliberto N, Nsouli A, Davis C, Cofsky K, Bellanti J (2016). "P162 The allergist, chronic cough and upper airway cough syndrome". Annals of Allergy, Asthma & Immunology. 117 (5): S70. doi:10.1016/j.anai.2016.09.173. ISSN 1081-1206.
- ↑ Tomerak AA, Vyas H, Lakenpaul M, McGlashan JJ, McKean M (July 2005). "Inhaled beta2-agonists for treating non-specific chronic cough in children". The Cochrane Database of Systematic Reviews. 2005 (3): CD005373. doi:10.1002/14651858.CD005373. PMC 8885309 . PMID 16034971.
- ↑ Tomerak AA, McGlashan JJ, Vyas HH, McKean MC (October 2005). "Inhaled corticosteroids for non-specific chronic cough in children". The Cochrane Database of Systematic Reviews. 2005 (4): CD004231. doi:10.1002/14651858.CD004231.pub2. PMC 9040101 . PMID 16235355.
- ↑ Gardiner SJ, Chang AB, Marchant JM, Petsky HL (July 2016). "Codeine versus placebo for chronic cough in children". The Cochrane Database of Systematic Reviews. 2016 (7): CD011914. doi:10.1002/14651858.CD011914.pub2. PMC 6457872 . PMID 27405706.
- ↑ Chang AB, Winter D, Acworth JP (April 2006). Chang AB (ed.). "Leukotriene receptor antagonist for prolonged non-specific cough in children". The Cochrane Database of Systematic Reviews. 2006 (2): CD005602. doi:10.1002/14651858.CD005602.pub2. PMC 8896275 . PMID 16625643.
- ↑ Chang AB, Halstead RA, Petsky HL (July 2005). "Methylxanthines for prolonged non-specific cough in children". The Cochrane Database of Systematic Reviews. 2005 (3): CD005310. doi:10.1002/14651858.CD005310.pub2. PMC 6823234 . PMID 16034969.
- ↑ McCallum GB, Bailey EJ, Morris PS, Chang AB (September 2014). "Clinical pathways for chronic cough in children". The Cochrane Database of Systematic Reviews (9): CD006595. doi:10.1002/14651858.CD006595.pub3. PMC 10640710 . PMID 25242448.
- ↑ Teoh L, Hurwitz M, Acworth JP, van Asperen P, Chang AB (April 2011). "Treatment of obstructive sleep apnoea for chronic cough in children". The Cochrane Database of Systematic Reviews (4): CD008182. doi:10.1002/14651858.CD008182.pub2. PMID 21491406.
- ↑ Donnelly D, Everard MM, Chang AB (July 2006). "Indoor air modification interventions for prolonged non-specific cough in children". The Cochrane Database of Systematic Reviews (3): CD005075. doi:10.1002/14651858.CD005075.pub2. PMID 16856075.
- ↑ Chang A, Marchant JM, McKean M, Morris P (2004). "Inhaled cromones for prolonged non-specific cough in children". The Cochrane Database of Systematic Reviews. 2004 (2): CD004436. doi:10.1002/14651858.CD004436.pub2. PMC 9036945 . PMID 15106252.
- 1 2 3 Chung KF, Pavord ID (April 2008). "Prevalence, pathogenesis, and causes of chronic cough". Lancet. 371 (9621): 1364–1374. doi:10.1016/s0140-6736(08)60595-4. PMID 18424325. S2CID 7810980.
- ↑ Abozid, Hazim; Patel, Jaymini; Burney, Peter; Hartl, Sylvia; Breyer-Kohansal, Robab; Mortimer, Kevin; Nafees, Asaad A.; Al Ghobain, Mohammed; Welte, Tobias; Harrabi, Imed; Denguezli, Meriam; Loh, Li Cher; Rashid, Abdul; Gislason, Thorarinn; Barbara, Cristina; Cardoso, Joao; Rodrigues, Fatima; Seemungal, Terence; Obaseki, Daniel; Juvekar, Sanjay; Paraguas, Stefanni Nonna; Tan, Wan C.; Franssen, Frits M. E.; Mejza, Filip; Mannino, David; Janson, Christer; Cherkaski, Hamid Hacene; Anand, Mahesh Padukudru; Hafizi, Hasan; Buist, Sonia; Koul, Parvaiz A.; El Sony, Asma; Breyer, Marie-Kathrin; Burghuber, Otto C.; Wouters, Emiel F. M.; Amaral, Andre F. S. (1 February 2024). "Prevalence of chronic cough, its risk factors and population attributable risk in the Burden of Obstructive Lung Disease (BOLD) study: a multinational cross-sectional study". eClinicalMedicine. 68: 102423. doi:10.1016/j.eclinm.2024.102423. ISSN 2589-5370. PMC 10807979 .
- ↑ Chang AB, Oppenheimer JJ, Weinberger MM, Rubin BK, Weir K, Grant CC, Irwin RS (April 2017). "Use of Management Pathways or Algorithms in Children With Chronic Cough: CHEST Guideline and Expert Panel Report". Chest. 151 (4): 875–883. doi: 10.1016/j.chest.2016.12.025 . PMID 28104362. S2CID 10306352.
- ↑ Singh D, Arora V, Sobti PC (January 2002). "Chronic/recurrent cough in rural children in Ludhiana, Punjab". Indian Pediatrics. 39 (1): 23–29. PMID 11805350.
- ↑ Flynn MG (August 1994). "Respiratory symptoms, bronchial responsiveness, and atopy in Fijian and Indian children". American Journal of Respiratory and Critical Care Medicine. 150 (2): 415–420. doi:10.1164/ajrccm.150.2.8049824. PMID 8049824.