Related Research Articles
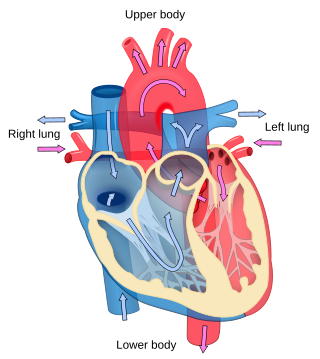
Cardiology is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.

Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in a brachial artery, where it is most commonly measured. Blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure, or in kilopascals (kPa). The difference between the systolic and diastolic pressures is known as pulse pressure, while the average pressure during a cardiac cycle is known as mean arterial pressure.

Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms itself. It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia. Hypertension is a major cause of premature death worldwide.
A hypertensive urgency is a clinical situation in which blood pressure is very high with minimal or no symptoms, and no signs or symptoms indicating acute organ damage. This contrasts with a hypertensive emergency where severely high blood pressure is accompanied by evidence of progressive organ or system damage.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.
Essential hypertension is a form of hypertension without an identifiable physiologic cause. It is the most common type affecting 85% of those with high blood pressure. The remaining 15% is accounted for by various causes of secondary hypertension. Essential hypertension tends to be familial and is likely to be the consequence of an interaction between environmental and genetic factors. Hypertension can increase the risk of cerebral, cardiac, and renal events.

Thiazide refers to both a class of sulfur-containing organic molecules and a class of diuretics based on the chemical structure of benzothiadiazine. The thiazide drug class was discovered and developed at Merck and Co. in the 1950s. The first approved drug of this class, chlorothiazide, was marketed under the trade name Diuril beginning in 1958. In most countries, thiazides are the least expensive antihypertensive drugs available.
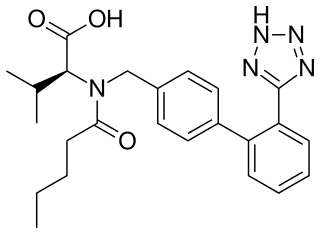
Valsartan, sold under the brand name Diovan among others, is a medication used to treat high blood pressure, heart failure, and diabetic kidney disease. It belongs to a class of medications referred to as angiotensin II receptor blockers (ARBs). It is a reasonable initial treatment for high blood pressure. It is taken by mouth.

A hypertensive emergency is very high blood pressure with potentially life-threatening symptoms and signs of acute damage to one or more organ systems. It is different from a hypertensive urgency by this additional evidence for impending irreversible hypertension-mediated organ damage (HMOD). Blood pressure is often above 200/120 mmHg, however there are no universally accepted cutoff values.
Secondary hypertension is a type of hypertension which by definition is caused by an identifiable underlying primary cause. It is much less common than the other type, called essential hypertension, affecting only 5-10% of hypertensive patients. It has many different causes including endocrine diseases, kidney diseases, and tumors. The cause of secondary hypertension varies significantly with age. It also can be a side effect of many medications.

Hypertensive heart disease includes a number of complications of high blood pressure that affect the heart. While there are several definitions of hypertensive heart disease in the medical literature, the term is most widely used in the context of the International Classification of Diseases (ICD) coding categories. The definition includes heart failure and other cardiac complications of hypertension when a causal relationship between the heart disease and hypertension is stated or implied on the death certificate. In 2013 hypertensive heart disease resulted in 1.07 million deaths as compared with 630,000 deaths in 1990.
Arterial stiffness occurs as a consequence of biological aging and arteriosclerosis. Inflammation plays a major role in arteriosclerosis development, and consequently it is a major contributor in large arteries stiffening. Increased arterial stiffness is associated with an increased risk of cardiovascular events such as myocardial infarction, hypertension, heart failure and stroke, the two leading causes of death in the developed world. The World Health Organization predicts that in 2010, cardiovascular disease will also be the leading killer in the developing world and represents a major global health problem.
In medicine, systolic hypertension is defined as an elevated systolic blood pressure (SBP). If the systolic blood pressure is elevated (>140) with a normal (<90) diastolic blood pressure (DBP), it is called isolated systolic hypertension. Eighty percent of people with systolic hypertension are over the age of 65 years old. Isolated systolic hypertension is a specific type of widened pulse pressure.

Intima–media thickness (IMT), also called intimal medial thickness, is a measurement of the thickness of tunica intima and tunica media, the innermost two layers of the wall of an artery. The measurement is usually made by external ultrasound and occasionally by internal, invasive ultrasound catheters. Measurements of the total wall thickness of blood vessels can also be done using other imaging modalities.
Prehypertension, also known as high normal blood pressure and borderline hypertensive (BH), is a medical classification for cases where a person's blood pressure is elevated above optimal or normal, but not to the level considered hypertension. Prehypertension is now referred to as "elevated blood pressure" by the American College of Cardiology (ACC) and the American Heart Association (AHA). The ACC/AHA define elevated blood pressure as readings with a systolic pressure from 120 to 129 mm Hg and a diastolic pressure under 80 mm Hg, Readings greater than or equal to 130/80 mm Hg are considered hypertension by ACC/AHA and if greater than or equal to 140/90 mm Hg by ESC/ESH. and the European Society of Hypertension defines "high normal blood pressure" as readings with a systolic pressure from 130 to 139 mm Hg and a diastolic pressure 85-89 mm Hg.
Central aortic blood pressure is the blood pressure at the root of aorta. Studies have shown the importance of central aortic pressure, especially as compared to peripheral blood pressure, and its implications in assessing the efficacy of antihypertensive treatment with respect to cardiovascular risk factors, kidney disease, and mortality. There is an emerging movement for clinicians to begin using central aortic blood pressure, instead of peripheral blood pressure, as a guide for clinical decisions.

Orthostatic hypertension is a medical condition consisting of a sudden and abrupt increase in blood pressure (BP) when a person stands up. Orthostatic hypertension is diagnosed by a rise in systolic BP of 20 mmHg or more when standing. Orthostatic diastolic hypertension is a condition in which the diastolic BP raises to 98 mmHg or over in response to standing, but this definition currently lacks clear medical consensus, so is subject to change. Orthostatic hypertension involving the systolic BP is known as systolic orthostatic hypertension.

Arterial blood pressure is most commonly measured via a sphygmomanometer, which historically used the height of a column of mercury to reflect the circulating pressure. Blood pressure values are generally reported in millimetres of mercury (mmHg), though aneroid and electronic devices do not contain mercury.
Hypertension is managed using lifestyle modification and antihypertensive medications. Hypertension is usually treated to achieve a blood pressure of below 140/90 mmHg to 160/100 mmHg. According to one 2003 review, reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21% and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease.
non-pharmacological intervention (NPI) is any type of healthcare intervention which is not primarily based on medication. Some examples include exercise, sleep improvement, and dietary habits.
References
- 1 2 James, PA.; Oparil, S.; Carter, BL.; Cushman, WC.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, DT.; Lefevre, ML.; Mackenzie, TD.; Ogedegbe, Olugbenga; Smith, Sidney C.; Svetkey, Laura P.; Taler, Sandra J.; Townsend, Raymond R.; Wright, Jackson T.; Narva, Andrew S.; Ortiz, Eduardo (Dec 2013). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8)". JAMA. 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
- ↑ Mancia, Giuseppe; Kreutz, Reinhold; Brunström, Mattias; Burnier, Michel; Grassi, Guido; et al. (2023-12-01). "2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA)". Journal of Hypertension. 41 (12): 1874–2071. doi: 10.1097/HJH.0000000000003480 . ISSN 1473-5598. PMID 37345492.
- ↑ Coles, Sarah; Fisher, Lynn; Lin, Kenneth W.; Lyon, Corey; Vosooney, Alexis A.; Bird, Melanie D. (December 2022). "Blood Pressure Targets in Adults With Hypertension: A Clinical Practice Guideline From the AAFP". American Family Physician. 106 (6): Online. ISSN 1532-0650. PMID 36521481.
- ↑ Clarke, S. Lindsey (October 2023). "Hypertension in Adults: Initial Evaluation and Management". American Family Physician. 108 (4): 352–359. ISSN 1532-0650. PMID 37843942.
- ↑ Guideline for the pharmacological treatment of hypertension in adults (PDF). World Health Organization (WHO). 2021. ISBN 9789240033993 . Retrieved 2024-05-26.
- ↑ Cheung, Alfred K.; Chang, Tara I.; Cushman, William C.; Furth, Susan L.; Hou, Fan Fan; Ix, Joachim H.; Knoll, Gregory A.; Muntner, Paul; Pecoits-Filho, Roberto; Sarnak, Mark J.; Tobe, Sheldon W.; Tomson, Charles R.V.; Mann, Johannes F.E. (March 2021). "KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease". Kidney International. 99 (3): S1–S87. doi: 10.1016/j.kint.2020.11.003 .
- ↑ Unger, Thomas; Borghi, Claudio; Charchar, Fadi; Khan, Nadia A.; Poulter, Neil R.; et al. (2020-05-06). "2020 International Society of Hypertension Global Hypertension Practice Guidelines". Hypertension. 75 (6): 1334–1357. doi: 10.1161/HYPERTENSIONAHA.120.15026 . ISSN 0194-911X.
- ↑ U.S. Department of Veterans Affairs. "VA/DoD clinical practice guideline for the diagnosis and management of hypertension in the primary care setting". VA/DoD Clinical Practice Guidelines. Retrieved 2024-03-25.
- ↑ "Hypertension in adults: diagnosis and management |". National Institute for Health and Clinical Excellence (NICE). 2019-08-28. Retrieved 2024-03-24.
- ↑ Passarella, Pasquale; Kiseleva, Tatiana A.; Valeeva, Farida V.; Gosmanov, Aidar R. (2018-08-01). "Hypertension Management in Diabetes: 2018 Update". Diabetes Spectrum. 31 (3): 218–224. doi:10.2337/ds17-0085. ISSN 1040-9165. PMC 6092891 . PMID 30140137.
- ↑ Williams, Bryan; Mancia, Giuseppe; Spiering, Wilko; Agabiti Rosei, Enrico; Azizi, Michel; et al. (1 September 2018). "2018 ESC/ESH Guidelines for the management of arterial hypertension". European Heart Journal. 39 (33): 3021–3104. doi:10.1093/eurheartj/ehy339. PMID 30165516.
- ↑ Whelton, Paul K.; Carey, Robert M.; Aronow, Wilbert S.; Casey, Donald E.; Collins, Karen J.; Dennison Himmelfarb, Cheryl; DePalma, Sondra M.; Gidding, Samuel; Jamerson, Kenneth A.; Jones, Daniel W.; MacLaughlin, Eric J.; Muntner, Paul; Ovbiagele, Bruce; Smith, Sidney C.; Spencer, Crystal C. (2018-05-15). "2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults". Journal of the American College of Cardiology. 71 (19): e127–e248. doi:10.1016/j.jacc.2017.11.006. PMID 29146535.
- ↑ Flack, John M.; Sica, Domenic A.; Bakris, George; Brown, Angela L.; Ferdinand, Keith C.; Grimm, Richard H.; Hall, W. Dallas; Jones, Wendell E.; Kountz, David S.; Lea, Janice P.; Nasser, Samar; Nesbitt, Shawna D.; Saunders, Elijah; Scisney-Matlock, Margaret; Jamerson, Kenneth A. (November 2010). "Management of High Blood Pressure in Blacks: An Update of the International Society on Hypertension in Blacks Consensus Statement". Hypertension. 56 (5): 780–800. doi:10.1161/HYPERTENSIONAHA.110.152892. ISSN 0194-911X.