A zoonosis or zoonotic disease is an infectious disease of humans caused by a pathogen that can jump from a non-human to a human and vice versa.

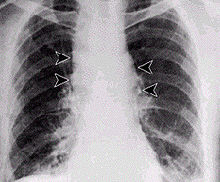
An epidemic is the rapid spread of disease to a large number of hosts in a given population within a short period of time. For example, in meningococcal infections, an attack rate in excess of 15 cases per 100,000 people for two consecutive weeks is considered an epidemic.
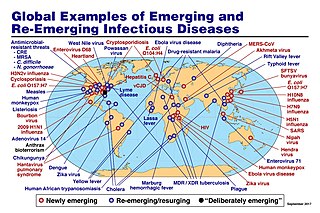
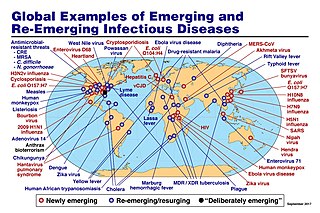
An emerging infectious disease (EID) is an infectious disease whose incidence has increased recently, and could increase in the near future. The minority that are capable of developing efficient transmission between humans can become major public and global concerns as potential causes of epidemics or pandemics. Their many impacts can be economic and societal, as well as clinical. EIDs have been increasing steadily since at least 1940.
Clarence James Peters, Jr is a physician, field virologist and former U.S. Army colonel. He is noted for his efforts in trying to stem epidemics of exotic infectious diseases such as the Ebola virus, Hanta virus and Rift Valley fever (RVF). He is an eminent authority on the virology, pathogenesis and epidemiology of hemorrhagic fever viruses.

The Biomedical Advanced Research and Development Authority (BARDA)' is a U.S. Department of Health and Human Services (HHS) office responsible for the procurement and development of medical countermeasures, principally against bioterrorism, including chemical, biological, radiological and nuclear (CBRN) threats, as well as pandemic influenza and emerging diseases. BARDA was established in 2006 through the Pandemic and All-Hazards Preparedness Act (PAHPA) and reports to the Office of the Assistant Secretary for Preparedness and Response (ASPR). The office manages Project BioShield, which funds the research, development and stockpiling of vaccines and treatments that the government could use during public health emergencies such as chemical, biological, radiological or nuclear (CBRN) attacks.

Walter Ian Lipkin is the John Snow Professor of Epidemiology at the Mailman School of Public Health at Columbia University and a professor of Neurology and Pathology at the College of Physicians and Surgeons at Columbia University. He is also director of the Center for Infection and Immunity, an academic laboratory for microbe hunting in acute and chronic diseases. Lipkin is internationally recognized for his work with West Nile virus, SARS and COVID-19.

The Vaccine Research Center (VRC), is an intramural division of the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH), US Department of Health and Human Services (HHS). The mission of the VRC is to discover and develop both vaccines and antibody-based products that target infectious diseases.

Luciana Borio is a Brazilian-American infectious disease physician and public health administrator. She is a vice president at In-Q-Tel. She previously served as director for Medical and Biodefense Preparedness at the National Security Council, acting chief scientist of the U.S. Food and Drug Administration (FDA), assistant commissioner for counterterrorism policy of the FDA, and director of FDA's Office of Counterterrorism and Emerging Threats. She is known for her work advancing clinical trials, the development of medical countermeasures for health emergencies, and the public health responses to Ebola and Zika outbreaks.

A public health emergency of international concern is a formal declaration by the World Health Organization (WHO) of "an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response", formulated when a situation arises that is "serious, sudden, unusual, or unexpected", which "carries implications for public health beyond the affected state's national border" and "may require immediate international action". Under the 2005 International Health Regulations (IHR), states have a legal duty to respond promptly to a PHEIC. The declaration is publicized by an IHR Emergency Committee (EC) of international experts, which was developed following the 2002–2004 SARS outbreak.
John Brownstein is a Canadian epidemiologist and Professor of Medicine at the Harvard Medical School as well as the Chief Innovation Officer at Boston Children’s Hospital. His research focuses on development of computational methods in epidemiology for applications to public health also known as computational epidemiology or e-epidemiology He is also the founder of several global public health surveillance systems including HealthMap. He is most known for his work on global tracking of disease outbreaks.

The Coalition for Epidemic Preparedness Innovations (CEPI) is a foundation that takes donations from public, private, philanthropic, and civil society organisations, to finance independent research projects to develop vaccines against emerging infectious diseases (EID).
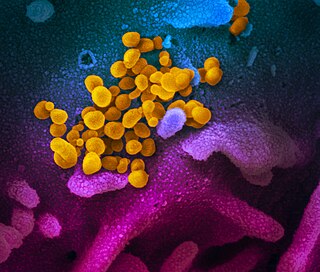
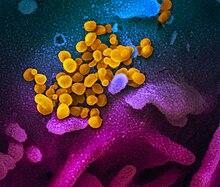
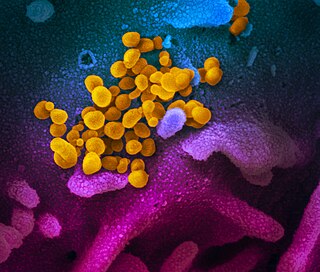
Disease X is a placeholder name that was adopted by the World Health Organization (WHO) in February 2018 on their shortlist of blueprint priority diseases to represent a hypothetical, unknown pathogen that could cause a future epidemic. The WHO adopted the placeholder name to ensure that their planning was sufficiently flexible to adapt to an unknown pathogen. Director of the US National Institute of Allergy and Infectious Diseases Anthony Fauci stated that the concept of Disease X would encourage WHO projects to focus their research efforts on entire classes of viruses, instead of just individual strains, thus improving WHO capability to respond to unforeseen strains. In 2020, experts, including some of the WHO's own expert advisors, speculated that COVID-19, caused by the SARS-CoV-2 virus strain, met the requirements to be the first Disease X.

Deadliest Enemy: Our War Against Killer Germs is a non-fiction book by epidemiologist Michael T. Osterholm and writer Mark Olshaker, that explores public health emergencies including antimicrobial resistance, emerging infectious disease, and the threat of an influenza pandemic. It proposes a nine-point "battle plan for survival" for dealing with these threats, including solutions to antimicrobial drug resistance.

Neil Morris Ferguson is a British epidemiologist and professor of mathematical biology, who specialises in the patterns of spread of infectious disease in humans and animals. He is the director of the Jameel Institute, and of the MRC Centre for Global Infectious Disease Analysis, and head of the Department of Infectious Disease Epidemiology in the School of Public Health and Vice-Dean for Academic Development in the Faculty of Medicine, all at Imperial College London.

Michael Joseph Ryan is an Irish epidemiologist and former trauma surgeon, specialising in infectious disease and public health. He is executive director of the World Health Organization's Health Emergencies Programme, leading the team responsible for the international containment and treatment of COVID-19. Ryan has held leadership positions and has worked on various outbreak response teams in the field to eradicate the spread of diseases including bacillary dysentery, cholera, Crimean–Congo hemorrhagic fever, Ebola, Marburg virus disease, measles, meningitis, relapsing fever, Rift Valley fever, SARS, and Shigellosis.
Trudie Lang is a Professor of Global Health Research at the University of Oxford. She specialises in clinical trials research capacity building in low-resource setting, and helped to organise the trial for the drug brincidofovir during the 2014 Ebola virus outbreak.

Caitlin M. Rivers is an American epidemiologist who as Senior Scholar at the Johns Hopkins Center for Health Security and assistant professor at the Johns Hopkins Bloomberg School of Public Health, specializing on improving epidemic preparedness. Rivers is currently working on the American response to the COVID-19 pandemic with a focus on the incorporation of infectious disease modeling and forecasting into public health decision making.
Peter Daszak is a British zoologist, consultant and public expert on disease ecology, in particular on zoonosis. He is the president of EcoHealth Alliance, a nonprofit non-governmental organization that supports various programs on global health and pandemic prevention. He is also a member of the Center for Infection and Immunity at the Columbia University Mailman School of Public Health. He lives in Suffern, New York.
Natalie E. Dean is an American biostatistician specializing in infectious disease epidemiology. Dean is currently an assistant professor of Biostatistics at the University of Florida. Her research involves epidemiological modeling of outbreaks, including Ebola, Zika and COVID-19.
Science diplomacy is the collaborative efforts by local and global entities to solve global issues using science and technology as a base. In science diplomacy, collaboration takes place to advance science but science can also be used to facilitate diplomatic relations. This allows even conflicting nations to come together through science to find solutions to global issues. Global organizations, researchers, public health officials, countries, government officials, and clinicians have previously worked together to create effective measures of infection control and subsequent treatment. They continue to do so through sharing of resources, research data, ideas, and by putting into effect laws and regulations that can further advance scientific research. Without the collaborative efforts of such entities, the world would not have the vaccines and treatments we now possess for diseases that were once considered deadly such as tuberculosis, tetanus, polio, influenza, etc. Historically, science diplomacy has proved successful in diseases such as SARS, Ebola, Zika and continues to be relevant during the COVID-19 pandemic today.