Related Research Articles
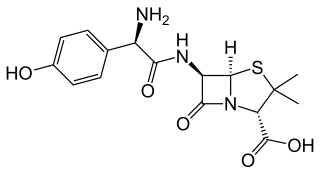
Amoxicillin is an antibiotic used to treat a number of bacterial infections. These include middle ear infection, strep throat, pneumonia, skin infections, and urinary tract infections among others. It is taken by mouth, or less commonly by injection.

Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of atherosclerotic plaque in the arteries of the heart. It is the most common of the cardiovascular diseases. Types include stable angina, unstable angina, myocardial infarction, and sudden cardiac death. A common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw. Occasionally it may feel like heartburn. Usually symptoms occur with exercise or emotional stress, last less than a few minutes, and improve with rest. Shortness of breath may also occur and sometimes no symptoms are present. In many cases, the first sign is a heart attack. Other complications include heart failure or an abnormal heartbeat.

Endocarditis is an inflammation of the inner layer of the heart, the endocardium. It usually involves the heart valves. Other structures that may be involved include the interventricular septum, the chordae tendineae, the mural endocardium, or the surfaces of intracardiac devices. Endocarditis is characterized by lesions, known as vegetations, which is a mass of platelets, fibrin, microcolonies of microorganisms, and scant inflammatory cells. In the subacute form of infective endocarditis, the vegetation may also include a center of granulomatous tissue, which may fibrose or calcify.

Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where they help keep the bite area unclotted long enough for the animal to obtain some blood. As a class of medications, anticoagulants are used in therapy for thrombotic disorders. Oral anticoagulants (OACs) are taken by many people in pill or tablet form, and various intravenous anticoagulant dosage forms are used in hospitals. Some anticoagulants are used in medical equipment, such as sample tubes, blood transfusion bags, heart–lung machines, and dialysis equipment. One of the first anticoagulants, warfarin, was initially approved as a rodenticide.

Aortic stenosis is the narrowing of the exit of the left ventricle of the heart, such that problems result. It may occur at the aortic valve as well as above and below this level. It typically gets worse over time. Symptoms often come on gradually with a decreased ability to exercise often occurring first. If heart failure, loss of consciousness, or heart related chest pain occur due to AS the outcomes are worse. Loss of consciousness typically occurs with standing or exercising. Signs of heart failure include shortness of breath especially when lying down, at night, or with exercise, and swelling of the legs. Thickening of the valve without narrowing is known as aortic sclerosis.
Bloodstream infections (BSIs), which include bacteremias when the infections are bacterial and fungemias when the infections are fungal, are infections present in the blood. Blood is normally a sterile environment, so the detection of microbes in the blood is always abnormal. A bloodstream infection is different from sepsis, which is the host response to bacteria.

Mitral valve prolapse (MVP) is a valvular heart disease characterized by the displacement of an abnormally thickened mitral valve leaflet into the left atrium during systole. It is the primary form of myxomatous degeneration of the valve. There are various types of MVP, broadly classified as classic and nonclassic. In severe cases of classic MVP, complications include mitral regurgitation, infective endocarditis, congestive heart failure, and, in rare circumstances, cardiac arrest.

Infective endocarditis is an infection of the inner surface of the heart, usually the valves. Signs and symptoms may include fever, small areas of bleeding into the skin, heart murmur, feeling tired, and low red blood cell count. Complications may include backward blood flow in the heart, heart failure – the heart struggling to pump a sufficient amount of blood to meet the body's needs, abnormal electrical conduction in the heart, stroke, and kidney failure.

Aortic regurgitation (AR), also known as aortic insufficiency (AI), is the leaking of the aortic valve of the heart that causes blood to flow in the reverse direction during ventricular diastole, from the aorta into the left ventricle. As a consequence, the cardiac muscle is forced to work harder than normal.

A congenital heart defect (CHD), also known as a congenital heart anomaly and congenital heart disease, is a defect in the structure of the heart or great vessels that is present at birth. A congenital heart defect is classed as a cardiovascular disease. Signs and symptoms depend on the specific type of defect. Symptoms can vary from none to life-threatening. When present, symptoms may include rapid breathing, bluish skin (cyanosis), poor weight gain, and feeling tired. CHD does not cause chest pain. Most congenital heart defects are not associated with other diseases. A complication of CHD is heart failure.

A medical guideline is a document with the aim of guiding decisions and criteria regarding diagnosis, management, and treatment in specific areas of healthcare. Such documents have been in use for thousands of years during the entire history of medicine. However, in contrast to previous approaches, which were often based on tradition or authority, modern medical guidelines are based on an examination of current evidence within the paradigm of evidence-based medicine. They usually include summarized consensus statements on best practice in healthcare. A healthcare provider is obliged to know the medical guidelines of his or her profession, and has to decide whether to follow the recommendations of a guideline for an individual treatment.

Acute coronary syndrome (ACS) is a syndrome due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally located chest pain, often radiating to the left shoulder or angle of the jaw, crushing, central and associated with nausea and sweating. Many people with acute coronary syndromes present with symptoms other than chest pain, particularly women, older people, and people with diabetes mellitus.
Antibiotic prophylaxis refers to, for humans, the prevention of infection complications using antimicrobial therapy. Antibiotic prophylaxis in domestic animal feed mixes has been employed in America since at least 1970.

Subacute bacterial endocarditis, abbreviated SBE, is a type of endocarditis. Subacute bacterial endocarditis can be considered a form of type III hypersensitivity.
Febrile neutropenia is the development of fever, often with other signs of infection, in a patient with neutropenia, an abnormally low number of neutrophil granulocytes in the blood. The term neutropenic sepsis is also applied, although it tends to be reserved for patients who are less well. In 50% of cases, an infection is detectable; bacteremia is present in approximately 20% of all patients with this condition.

Antibiotic misuse, sometimes called antibiotic abuse or antibiotic overuse, refers to the misuse or overuse of antibiotics, with potentially serious effects on health. It is a contributing factor to the development of antibiotic resistance, including the creation of multidrug-resistant bacteria, informally called "super bugs": relatively harmless bacteria can develop resistance to multiple antibiotics and cause life-threatening infections.
Evidence-based dentistry (EBD) is the dental part of the more general movement toward evidence-based medicine and other evidence-based practices. The pervasive access to information on the internet includes different aspects of dentistry for both the dentists and patients. This has created a need to ensure that evidence referenced to are valid, reliable and of good quality.
There are many circumstances during dental treatment where antibiotics are prescribed by dentists to prevent further infection. The most common antibiotic prescribed by dental practitioners is penicillin in the form of amoxicillin, however many patients are hypersensitive to this particular antibiotic. Therefore, in the cases of allergies, erythromycin is used instead.
Percutaneous pulmonary valve implantation (PPVI), also known as transcatheter pulmonary valve replacement (TPVR), is the replacement of the pulmonary valve via catheterization through a vein. It is a significantly less invasive procedure in comparison to open heart surgery and is commonly used to treat conditions such as pulmonary atresia.
Granulicatella adiacens is a fastidious Gram-positive cocci and is part of the nutritionally variant streptococci (NVS). Like other constituents of the NVS, it can cause bacteremia and infective endocarditis (IE), with significant morbidity and mortality. NVS has less often been implicated in a variety of other infections, including those of the orbit, nasolacrimal duct and breast implants. It is a commensal of the human mouth, genital, and intestinal tracts, although it is rarely implicated in infections, in part due to it being a fastidious organism and rarely being identified in the laboratory environment. However, its identification has become more frequent with use of commercial mediums and automated identification systems. Because it has been difficult to identify, it has been considered one of the causes of culture negative IE. Identifying G. adiacens can allow more appropriate selection of antibiotics, especially when susceptibility testing is not available.
References
- 1 2 Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, et al. (October 2007). "Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group". Circulation. 116 (15): 1736–54. doi: 10.1161/CIRCULATIONAHA.106.183095 . PMID 17446442.
- ↑ Zadik Y, Findler M, Livne S, Levin L, Elad S (December 2008). "Dentists' knowledge and implementation of the 2007 American Heart Association guidelines for prevention of infective endocarditis". Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 106 (6): e16-9. doi:10.1016/j.tripleo.2008.08.009. PMID 19000604.
- ↑ Elad S, Binenfeld-Alon E, Zadik Y, Aharoni M, Findler M (March 2011). "Survey of acceptance of the 2007 American Heart Association guidelines for the prevention of infective endocarditis: a pilot study". Quintessence International. 42 (3): 243–51. PMID 21465012.
- ↑ Lockhart PB, Loven B, Brennan MT, Fox PC (April 2007). "The evidence base for the efficacy of antibiotic prophylaxis in dental practice". Journal of the American Dental Association. 138 (4): 458–74, quiz 534–5, 437. doi:10.14219/jada.archive.2007.0198. PMID 17403736. S2CID 28694677.
- 1 2 3 4 5 6 "Antibiotic Prophylaxis Against Infective Endocarditis Implementation Advice" (PDF). Scottish Dental Clinical Effectiveness Programme (SDCEP). August 2018.
- ↑ McDonald JR (September 2009). "Acute infective endocarditis". Infectious Disease Clinics of North America. 23 (3): 643–64. doi:10.1016/j.idc.2009.04.013. PMC 2726828 . PMID 19665088.
- ↑ Delahaye F, M'Hammedi A, Guerpillon B, de Gevigney G, Boibieux A, Dauwalder O, et al. (January 2016). "Systematic Search for Present and Potential Portals of Entry for Infective Endocarditis". Journal of the American College of Cardiology. 67 (2): 151–158. doi: 10.1016/j.jacc.2015.10.065 . PMID 26791061.
- ↑ Duval X, Alla F, Hoen B, Danielou F, Larrieu S, Delahaye F, et al. (June 2006). "Estimated risk of endocarditis in adults with predisposing cardiac conditions undergoing dental procedures with or without antibiotic prophylaxis". Clinical Infectious Diseases. 42 (12): e102-7. doi: 10.1086/504385 . PMID 16705565.
- ↑ Tubiana S, Blotière PO, Hoen B, Lesclous P, Millot S, Rudant J, et al. (September 2017). "Dental procedures, antibiotic prophylaxis, and endocarditis among people with prosthetic heart valves: nationwide population based cohort and a case crossover study". BMJ. 358: j3776. doi:10.1136/bmj.j3776. PMC 5588045 . PMID 28882817.
- ↑ British National Formulary (75th ed.). London: BMJ Group and Pharmaceutical Press. 18 December 2018.
- ↑ "Drug Prescribing for Dentistry". Scottish Dental Clinical Effectiveness Programme (SDCEP) (3rd ed.). Retrieved 2019-02-13.
- ↑ Rutherford, Samantha J.; Glenny, Anne-Marie; Roberts, Graham; Hooper, Lee; Worthington, Helen V. (2022-05-10). "Antibiotic prophylaxis for preventing bacterial endocarditis following dental procedures". The Cochrane Database of Systematic Reviews. 5: CD003813. doi:10.1002/14651858.CD003813.pub5. ISSN 1469-493X. PMC 9088886 . PMID 35536541.
- ↑ Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. (November 2015). "2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM)". European Heart Journal. 36 (44): 3075–3128. doi: 10.1093/eurheartj/ehv319 . PMID 26320109.
- ↑ Prevention and Management of Dental Caries in Children. Scottish Dental Clinical Effectiveness Programme Guidelines (2nd ed.). 17 August 2018.