The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

Exocrine glands are glands that secrete substances onto an epithelial surface by way of a duct. Examples of exocrine glands include sweat, salivary, mammary, ceruminous, lacrimal, sebaceous, prostate and mucous. Exocrine glands are one of two types of glands in the human body, the other being endocrine glands, which secrete their products directly into the bloodstream. The liver and pancreas are both exocrine and endocrine glands; they are exocrine glands because they secrete products—bile and pancreatic juice—into the gastrointestinal tract through a series of ducts, and endocrine because they secrete other substances directly into the bloodstream. Exocrine sweat glands are part of the integumentary system; they have eccrine and apocrine types.

Chronic pancreatitis is a long-standing inflammation of the pancreas that alters the organ's normal structure and functions. It can present as episodes of acute inflammation in a previously injured pancreas, or as chronic damage with persistent pain or malabsorption. It is a disease process characterized by irreversible damage to the pancreas as distinct from reversible changes in acute pancreatitis. Tobacco smoke and alcohol misuse are two of the most frequently implicated causes, and the two risk factors are thought to have a synergistic effect with regards to the development of chronic pancreatitis. Chronic pancreatitis is a risk factor for the development of pancreatic cancer.

Digestive enzymes are a group of enzymes that break down polymeric macromolecules into their smaller building blocks, in order to facilitate their absorption into the cells of the body. Digestive enzymes are found in the digestive tracts of animals and in the tracts of carnivorous plants, where they aid in the digestion of food, as well as inside cells, especially in their lysosomes, where they function to maintain cellular survival. Digestive enzymes of diverse specificities are found in the saliva secreted by the salivary glands, in the secretions of cells lining the stomach, in the pancreatic juice secreted by pancreatic exocrine cells, and in the secretions of cells lining the small and large intestines.

Cystic fibrosis transmembrane conductance regulator (CFTR) is a membrane protein and anion channel in vertebrates that is encoded by the CFTR gene.
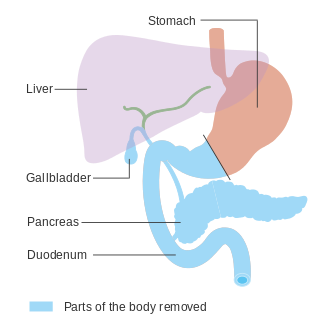
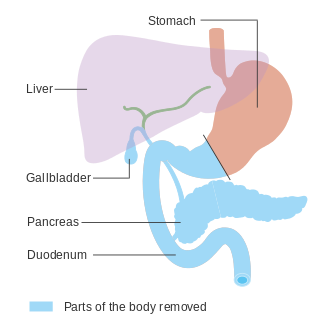
In medicine, a pancreatectomy is the surgical removal of all or part of the pancreas. Several types of pancreatectomy exist, including pancreaticoduodenectomy, distal pancreatectomy, segmental pancreatectomy, and total pancreatectomy. In recent years, the TP-IAT has also gained respectable traction within the medical community. These procedures are used in the management of several conditions involving the pancreas, such as benign pancreatic tumors, pancreatic cancer, and pancreatitis.
Pancreatic juice is a liquid secreted by the pancreas, which contains a number of digestive enzymes, including trypsinogen, chymotrypsinogen, elastase, carboxypeptidase, pancreatic lipase, nucleases and amylase. The pancreas is located in the visceral region, and is a major part of the digestive system required for proper digestion and subsequent assimilation of macronutrient substances required for living.

Exocrine pancreatic insufficiency (EPI) is the inability to properly digest food due to a lack or reduction of digestive enzymes made by the pancreas. EPI can occur in humans and is prevalent in many conditions such as cystic fibrosis, Shwachman–Diamond syndrome, different types of pancreatitis, multiple types of diabetes mellitus, advanced renal disease, older adults, celiac disease, IBS-D, IBD, HIV, alcohol-related liver disease, Sjogren syndrome, tobacco use, and use of somatostatin analogues.
Pancreatic diseases are diseases that affect the pancreas, an organ in most vertebrates and in humans and other mammals located in the abdomen. The pancreas plays a role in the digestive and endocrine system, producing enzymes which aid the digestion process and the hormone insulin, which regulates blood sugar levels. The most common pancreatic disease is pancreatitis, an inflammation of the pancreas which could come in acute or chronic form. Other pancreatic diseases include diabetes mellitus, exocrine pancreatic insufficiency, cystic fibrosis, pseudocysts, cysts, congenital malformations, tumors including pancreatic cancer, and hemosuccus pancreaticus.
Pancreatic elastase is a form of elastase that is produced in the acinar cells of the pancreas, initially produced as an inactive zymogen and later activated in the duodenum by trypsin. Elastases form a subfamily of serine proteases, characterized by a distinctive structure consisting of two beta barrel domains converging at the active site that hydrolyze amides and esters amongst many proteins in addition to elastin, a type of connective tissue that holds organs together. Pancreatic elastase 1 is a serine endopeptidase, a specific type of protease that has the amino acid serine at its active site. Although the recommended name is pancreatic elastase, it can also be referred to as elastase-1, pancreatopeptidase, PE, or serine elastase.

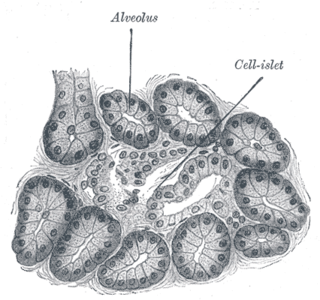
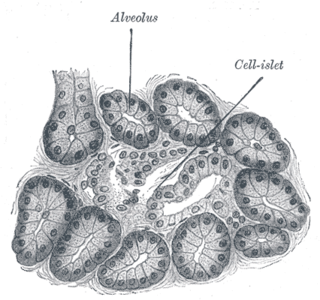
An acinus refers to any cluster of cells that resembles a many-lobed "berry," such as a raspberry. The berry-shaped termination of an exocrine gland, where the secretion is produced, is acinar in form, as is the alveolar sac containing multiple alveoli in the lungs.
The secretin-cholecystokinin test is a combination of the secretin test and the cholecystokinin test and is used to assess the function of both the pancreas and gall bladder.
Pancreatic stellate cells (PaSCs) are classified as myofibroblast-like cells that are located in exocrine regions of the pancreas. PaSCs are mediated by paracrine and autocrine stimuli and share similarities with the hepatic stellate cell. Pancreatic stellate cell activation and expression of matrix molecules constitute the complex process that induces pancreatic fibrosis. Synthesis, deposition, maturation and remodelling of the fibrous connective tissue can be protective, however when persistent it impedes regular pancreatic function.

Neurogenin-3 (NGN3) is a protein that in humans is encoded by the Neurog3 gene.
Canine pancreatitis is inflammation of the pancreas that can occur in two very different forms. Acute pancreatitis is sudden, while chronic pancreatitis is characterized by recurring or persistent form of pancreatic inflammation. Cases of both can be considered mild or severe.
Cystic fibrosis–related diabetes (CFRD) is diabetes specifically caused by cystic fibrosis, a genetic condition. Cystic fibrosis related diabetes mellitus (CFRD) develops with age, and the median age at diagnosis is 21 years. It is an example of type 3c diabetes – diabetes that is caused by damage to the pancreas from another disease or condition.

A pancreatic tumor is an abnormal growth in the pancreas. In adults, almost 90% are pancreatic cancer and a few are benign. Pancreatic tumors are rare in children.

The human digestive system consists of the gastrointestinal tract plus the accessory organs of digestion. Digestion involves the breakdown of food into smaller and smaller components, until they can be absorbed and assimilated into the body. The process of digestion has three stages: the cephalic phase, the gastric phase, and the intestinal phase.

Pancreatic progenitor cells are multipotent stem cells originating from the developing fore-gut endoderm which have the ability to differentiate into the lineage specific progenitors responsible for the developing pancreas.
Heterocrine glands are the glands which function as both exocrine gland and endocrine gland. These glands exhibit a unique and diverse secretory function encompassing the release of proteins and non-proteinaceous compounds, endocrine and exocrine secretions into both the bloodstream and ducts respectively, thereby bridging the realms of internal and external communication within the body. This duality allows them to serve crucial roles in regulating various physiological processes and maintaining homeostasis. These include the gonads, pancreas and salivary glands.