Related Research Articles

King's College Hospital is a major trauma centre in Denmark Hill, Camberwell in the London Borough of Lambeth, referred to locally and by staff simply as "King's" or abbreviated internally to "KCH". It is managed by King's College Hospital NHS Foundation Trust. It serves an inner city population of 700,000 in the London boroughs of Southwark and Lambeth, but also serves as a tertiary referral centre in certain specialties to millions of people in southern England. It is a large teaching hospital and is, with Guy's Hospital and St. Thomas' Hospital, the location of King's College London School of Medicine and one of the institutions that comprise the King's Health Partners, an academic health science centre. The chief executive is Dr Clive Kay.

The Royal London Hospital is a large teaching hospital in Whitechapel in the London Borough of Tower Hamlets. It is part of Barts Health NHS Trust. The Royal London provides district general hospital services for the City and Tower Hamlets and specialist tertiary care services for patients from across London and elsewhere. There are 845 beds, 110 wards and 26 operating theatres at the Royal London Hospital. The new building opened in February 2012.
The Orsan plan is the emergency plan in France to face a sudden increase of activity in a hospital, such as a massive arrival of casualties due to an accident or a disaster, an epidemic or a lasting climatic event that becomes deadly for fragile people such as a heatwave.
Health care in Ireland is delivered through public and private healthcare. The public health care system is governed by the Health Act 2004, which established a new body to be responsible for providing health and personal social services to everyone living in Ireland – the Health Service Executive. The new national health service came into being officially on 1 January 2005; however the new structures are currently in the process of being established as the reform programme continues. In addition to the public-sector, there is also a large private healthcare market.

Manchester Royal Infirmary is a hospital in Manchester, England, founded by Charles White in 1752. It is now part of Manchester University NHS Foundation Trust, sharing buildings and facilities with several other hospitals.

The National Disaster Medical System (NDMS) is a federally coordinated healthcare system and partnership of the United States Departments of Health and Human Services (HHS), Homeland Security (DHS), Defense (DOD), and Veterans Affairs (VA). The purpose of the NDMS is to support State, local, Tribal and Territorial authorities following disasters and emergencies by supplementing health and medical systems and response capabilities. NDMS would also support the military and the Department of Veterans Affairs health care systems in caring for combat casualties, should requirements exceed their capacity.

The Royal Voluntary Service is a voluntary organisation concerned with helping people in need throughout England, Scotland, Wales and Northern Ireland. It was founded in 1938 by Stella Isaacs, Marchioness of Reading, as a British women's organisation to recruit women into the Air Raid Precautions (ARP) services to help in the event of War.

The name National Health Service (NHS) is used to refer to the free public health services of England, Scotland and Wales, individually or collectively. Northern Ireland is known as 'Health and Social Care' to promote its dual integration of health and social services.
Hospital emergency codes are coded messages often announced over a public address system of a hospital to alert staff to various classes of on-site emergencies. The use of codes is intended to convey essential information quickly and with minimal misunderstanding to staff while preventing stress and panic among visitors to the hospital. Such codes are sometimes posted on placards throughout the hospital or are printed on employee identification badges for ready reference.
Dr David Stark Murray, son of Robert Murray MP was a consultant pathologist, author, and President of the Socialist Medical Association 1951–70. He was active in campaigning for the establishment of the British National Health Service.

Emergency medical services in the United Kingdom provide emergency care to people with acute illness or injury and are predominantly provided free at the point of use by the four National Health Services (NHS) of England, Scotland, Wales, and Northern Ireland. Emergency care including ambulance and emergency department treatment is only free to UK residents and a charge may be made to those not entitled to free NHS care. The NHS commissions most emergency medical services through the 14 NHS organisations with ambulance responsibility across the UK.

Soroka University Medical Center, part of the Clalit Health Services Group, is the general hospital of Beersheba, Israel, it serves as the central hospital of the region and provides medical services to approximately one million residents of the South, from Kiryat Gat and Ashkelon to Eilat. Soroka is the largest general hospital in Israel, with 1,151 hospital beds, and it is spread over an area of 291 dunams in the center of Beer-Sheva.
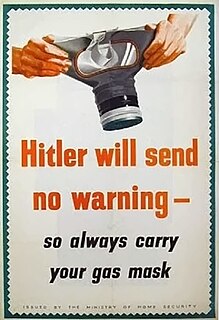
The Ministry of Home Security was a British government department established in 1939 to direct national civil defence, primarily tasked with organising air raid precautions, during the Second World War. The Ministry for Home Security was headed by Sir John Anderson, the Home Secretary and Minister of Home Security. The Ministry's responsibilities covered all central and regional civil defence organisations, such as air raid wardens, rescue squads, fire services, and the Women’s Voluntary Service. It was also responsible for giving approval to local ARP schemes and providing public shelters.

Stracathro Hospital is a community hospital in Angus, Scotland. Established as a wartime Emergency Hospital Service facility, it became a District General Hospital. Since 2005 it has been the site of the Scottish Regional Treatment Centre.

Lakeridge Health Ajax and Pickering is a hospital in Ajax, Ontario, Canada that is operated by Lakeridge Health. The hospital opened in 1954 as the Ajax and Pickering General Hospital.

Air medical services is a comprehensive term covering the use of air transportation, aeroplane or helicopter, to move patients to and from healthcare facilities and accident scenes. Personnel provide comprehensive prehospital and emergency and critical care to all types of patients during aeromedical evacuation or rescue operations aboard helicopter and propeller aircraft or jet aircraft.
Compared with other neighbouring countries, Guyana ranks poorly in regard to basic health indicators. Basic health services in the interior are primitive to non-existent, and some procedures are not available at all. Although Guyana's health profile falls short in comparison with many of its Caribbean neighbours, there has been remarkable progress since 1988, and the Ministry of Health is working to upgrade conditions, procedures, and facilities. Many Guyanese seek medical care in the United States, Trinidad and Tobago or Cuba.
The Emergency Hospital Service (EHS) of Scotland was an intensive, publicly funded programme of hospital building conducted by the Department of Health for Scotland during the 1940s. The scale and pace of public investment in hospital construction and staffing was unprecedented in Europe.
The King's Birthday Honours 1941 were appointments in the British Empire of King George VI to various orders and honours to reward and highlight good works by citizens of various countries. The appointments were made to celebrate the official birthday of The King, and were published on 6 June 1941.
Healthcare in London, which consumes about a fifth of the NHS budget in England, is in many respects distinct from that in the rest of the United Kingdom, or England.
References
- ↑ Paul Addison, "The Road to 1945", Jonathan Cape, 1975, pp. 178–81.
- ↑ Stark Murray, David (1942). Health For All. London: Gollancz. p. 28. Retrieved 28 August 2015.
- 1 2 Rivett, Geoffrey. "Emergency Medical Services - 1939-1945". NHS History. Retrieved 28 August 2015.
- 1 2 3 4 Titmuss, Richard. "Problems of Social Policy" . Retrieved 28 August 2015.
- 1 2 Timmins, Nicholas (1995). The Five Giants. London: Fontana. p. 103. ISBN 0006863183.
- ↑ Abel-Smith, Brian (1960). A History of the Nursing Profession. London: Heinemann. p. 161.
- ↑ Webster, Charles (1988). The Health Services Since the War. London: HMSO. p. 328. ISBN 0116309423.
- 1 2 Stark Murray, David (1942). Health For All. London: Gollancz. p. 29. Retrieved 28 August 2015.
- ↑ Brook, Charles (1943). "Memorandum on an Emergency Domiciliary Medical Service". Socialist Medical Association. Retrieved 28 August 2015.