Tinea cruris, also known as jock itch, is a common type of contagious, superficial fungal infection of the groin and buttocks region, which occurs predominantly but not exclusively in men and in hot-humid climates.

Folliculitis is the infection and inflammation of one or more hair follicles. The condition may occur anywhere on hair-covered skin. The rash may appear as pimples that come to white tips on the face, chest, back, arms, legs, buttocks, or head.

Athlete's foot, known medically as tinea pedis, is a common skin infection of the feet caused by a fungus. Signs and symptoms often include itching, scaling, cracking and redness. In rare cases the skin may blister. Athlete's foot fungus may infect any part of the foot, but most often grows between the toes. The next most common area is the bottom of the foot. The same fungus may also affect the nails or the hands. It is a member of the group of diseases known as tinea.
Dermatophyte is a common label for a group of fungus of Arthrodermataceae that commonly causes skin disease in animals and humans. Traditionally, these anamorphic mold genera are: Microsporum, Epidermophyton and Trichophyton. There are about 40 species in these three genera. Species capable of reproducing sexually belong in the teleomorphic genus Arthroderma, of the Ascomycota. As of 2019 a total of nine genera are identified and new phylogenetic taxonomy has been proposed.

Tinea corporis is a fungal infection of the body, similar to other forms of tinea. Specifically, it is a type of dermatophytosis that appears on the arms and legs, especially on glabrous skin; however, it may occur on any superficial part of the body.

Tinea capitis is a cutaneous fungal infection (dermatophytosis) of the scalp. The disease is primarily caused by dermatophytes in the genera Trichophyton and Microsporum that invade the hair shaft. The clinical presentation is typically single or multiple patches of hair loss, sometimes with a 'black dot' pattern, that may be accompanied by inflammation, scaling, pustules, and itching. Uncommon in adults, tinea capitis is predominantly seen in pre-pubertal children, more often boys than girls.

Dermatophytosis, also known as tinea and ringworm, is a fungal infection of the skin, that may affect skin, hair, and nails. Typically it results in a red, itchy, scaly, circular rash. Hair loss may occur in the area affected. Symptoms begin four to fourteen days after exposure. The types of dermatophytosis are typically named for area of the body that they affect. Multiple areas can be affected at a given time.

Kerion or kerion celsi is an acute inflammatory process which is the result of the host's response to a fungal ringworm infection of the hair follicles of the scalp that can be accompanied by secondary bacterial infection(s). It usually appears as raised, spongy lesions, and typically occurs in children. This honeycomb is a painful inflammatory reaction with deep suppurative lesions on the scalp. Follicles may be seen discharging pus. There may be sinus formation and rarely mycetoma-like grains are produced. It is usually caused by dermatophytes such as Trichophyton verrucosum, T. mentagrophytes, and Microsporum canis. Treatment with oral griseofulvin common.

Trichophyton rubrum is a dermatophytic fungus in the phylum Ascomycota. It is an exclusively clonal, anthropophilic saprotroph that colonizes the upper layers of dead skin, and is the most common cause of athlete's foot, fungal infection of nail, jock itch, and ringworm worldwide. Trichophyton rubrum was first described by Malmsten in 1845 and is currently considered to be a complex of species that comprises multiple, geographically patterned morphotypes, several of which have been formally described as distinct taxa, including T. raubitschekii, T. gourvilii, T. megninii and T. soudanense.

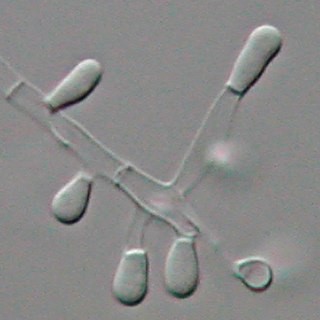
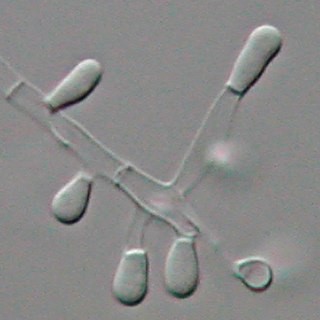
Trichophyton is a genus of fungi, which includes the parasitic varieties that cause tinea, including athlete's foot, ringworm, jock itch, and similar infections of the nail, beard, skin and scalp. Trichophyton fungi are molds characterized by the development of both smooth-walled macro- and microconidia. Macroconidia are mostly borne laterally directly on the hyphae or on short pedicels, and are thin- or thick-walled, clavate to fusiform, and range from 4 to 8 by 8 to 50 μm in size. Macroconidia are few or absent in many species. Microconidia are spherical, pyriform to clavate or of irregular shape, and range from 2 to 3 by 2 to 4 μm in size.

Microsporum audouinii is an anthropophilic fungus in the genus Microsporum. It is a type of dermatophyte that colonizes keratinized tissues causing infection. The fungus is characterized by its spindle-shaped macroconidia, clavate microconidia as well as its pitted or spiny external walls.
Trichophyton tonsurans is a fungus in the family Arthrodermataceae that causes ringworm infection of the scalp. It was first recognized by David Gruby in 1844. Isolates are characterized as the "–" or negative mating type of the Arthroderma vanbreuseghemii complex. This species is thought to be conspecific with T. equinum, although the latter represents the "+" mating strain of the same biological species Despite their biological conspecificity, clones of the two mating types appear to have undergone evolutionary divergence with isolates of the T. tonsurans-type consistently associated with Tinea capitis whereas the T. equinum-type, as its name implies, is associated with horses as a regular host. Phylogenetic relationships were established in isolates from Northern Brazil, through fingerprinting polymorphic RAPD and M13 markers. There seems to be lower genomic variability in the T. tonsurans species due to allopatric divergence. Any phenotypic density is likely due to environmental factors, not genetic characteristics of the fungus.

Trichophyton mentagrophytes is a species in the fungal genus Trichophyton. It is one of three common fungi which cause ringworm in companion animals. It is also the second-most commonly isolated fungus causing tinea infections in humans, and the most common or one of the most common fungi that cause zoonotic skin disease. Trichophyton mentagrophytes is being frequently isolated from dogs, cats, rabbits, guinea pigs and other rodents, though at least some genetic variants possess the potential of human-to-human transmission, e.g. Type VII and Type VIII. Particular genetic variants of the fungus have distinct geographic ranges.
Trichophyton concentricum is an anthropophilic dermatophyte believed to be an etiological agent of a type of skin mycosis in humans, evidenced by scaly cutaneous patches on the body known as tinea imbricata. This fungus has been found mainly in the Pacific Islands and South America.
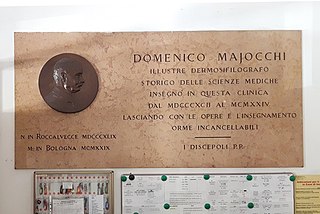
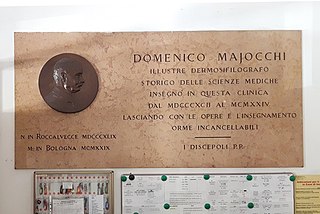
Domenico Majocchi (1849–1929) was an Italian dermatologist, an histologist and anatomo-pathologist of great value and an extremely expert clinician, who discovered some pathologies such as the purpura annularis telangiectodes and the Fungal folliculitis.

Aphanoascus fulvescens is a mould fungus that behaves as a keratinophilic saprotroph and belongs to the Ascomycota. It is readily isolated from soil and dung containing keratin-rich tissues that have been separated from their animal hosts. This organism, distributed worldwide, is most commonly found in areas of temperate climate, in keeping with its optimal growth temperature of 28 °C (82 °F). While A. fulvescens is recognized as a geophilic fungal species, it is also a facultative opportunistic pathogen. Although it is not a dermatophyte, A. fulvescens has occasionally been shown to cause onychomycosis infections in humans. Its recognition in the laboratory is clinically important for correct diagnosis and treatment of human dermal infections.

Microsporum gallinae is a fungus of the genus Microsporum that causes dermatophytosis, commonly known as ringworm. Chickens represent the host population of Microsporum gallinae but its opportunistic nature allows it to enter other populations of fowl, mice, squirrels, cats, dogs and monkeys. Human cases of M. gallinae are rare, and usually mild, non-life-threatening superficial infections.

Favus or tinea favosa is the severe form of tinea capitis, a skin infectious disease caused by the dermatophyte fungus Trichophyton schoenleinii. Typically the species affects the scalp, but occasionally occurs as onychomycosis, tinea barbae, or tinea corporis.

Epidermophyton floccosum is a filamentous fungus that causes skin and nail infections in humans. This anthropophilic dermatophyte can lead to diseases such as tinea pedis, tinea cruris, tinea corporis and onychomycosis. Diagnostic approaches of the fungal infection include physical examination, culture testing, and molecular detection. Topical antifungal treatment, such as the use of terbinafine, itraconazole, voriconazole, and ketoconazole, is often effective.