Related Research Articles

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.

Adrenoleukodystrophy (ALD) is a disease linked to the X chromosome. It is a result of fatty acid buildup caused by failure of peroxisomal fatty acid beta oxidation which results in the accumulation of very long chain fatty acids in tissues throughout the body. The most severely affected tissues are the myelin in the central nervous system, the adrenal cortex, and the Leydig cells in the testes. The long chain fatty acid buildup causes damage to the myelin sheath of the neurons of the brain, resulting in seizures and hyperactivity. Other symptoms include problems in speaking, listening, and understanding verbal instructions.
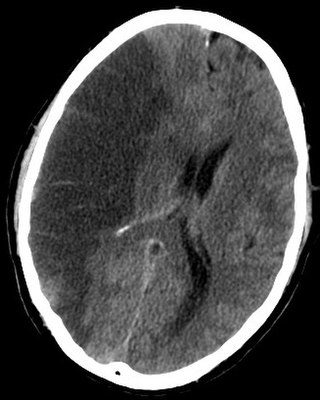
Porencephaly is an extremely rare cephalic disorder involving encephalomalacia. It is a neurological disorder of the central nervous system characterized by cysts or cavities within the cerebral hemisphere. Porencephaly was termed by Heschl in 1859 to describe a cavity in the human brain. Derived from Greek roots, the word porencephaly means 'holes in the brain'. The cysts and cavities are more likely to be the result of destructive (encephaloclastic) cause, but can also be from abnormal development (malformative), direct damage, inflammation, or hemorrhage. The cysts and cavities cause a wide range of physiological, physical, and neurological symptoms. Depending on the patient, this disorder may cause only minor neurological problems, without any disruption of intelligence, while others may be severely disabled or die before the second decade of their lives. However, this disorder is far more common within infants, and porencephaly can occur both before or after birth.

Carbon monoxide poisoning typically occurs from breathing in carbon monoxide (CO) at excessive levels. Symptoms are often described as "flu-like" and commonly include headache, dizziness, weakness, vomiting, chest pain, and confusion. Large exposures can result in loss of consciousness, arrhythmias, seizures, or death. The classically described "cherry red skin" rarely occurs. Long-term complications may include chronic fatigue, trouble with memory, and movement problems.
A demyelinating disease refers to any disease affecting the nervous system where the myelin sheath surrounding neurons is damaged. This damage disrupts the transmission of signals through the affected nerves, resulting in a decrease in their conduction ability. Consequently, this reduction in conduction can lead to deficiencies in sensation, movement, cognition, or other functions depending on the nerves affected.

Cerebral hypoxia is a form of hypoxia, specifically involving the brain; when the brain is completely deprived of oxygen, it is called cerebral anoxia. There are four categories of cerebral hypoxia; they are, in order of increasing severity: diffuse cerebral hypoxia (DCH), focal cerebral ischemia, cerebral infarction, and global cerebral ischemia. Prolonged hypoxia induces neuronal cell death via apoptosis, resulting in a hypoxic brain injury.

Leukodystrophies are a group of, usually, inherited disorders, characterized by degeneration of the white matter in the brain. The word leukodystrophy comes from the Greek roots leuko, "white", dys, "abnormal" and troph, "growth". The leukodystrophies are caused by imperfect growth or development of the glial cells which produce the myelin sheath, the fatty insulating covering around nerve fibers. Leukodystrophies may be classified as hypomyelinating or demyelinating diseases, respectively, depending on whether the damage is present before birth or occurs after. Other demyelinating diseases are usually not congenital and have a toxic or autoimmune cause.

Periventricular leukomalacia (PVL) is a form of white-matter brain injury, characterized by the necrosis of white matter near the lateral ventricles. It can affect newborns and fetuses; premature infants are at the greatest risk of neonatal encephalopathy which may lead to this condition. Affected individuals generally exhibit motor control problems or other developmental delays, and they often develop cerebral palsy or epilepsy later in life. The white matter in preterm born children is particularly vulnerable during the third trimester of pregnancy when white matter developing takes place and the myelination process starts around 30 weeks of gestational age.
Experimental autoimmune encephalomyelitis, sometimes experimental allergic encephalomyelitis (EAE), is an animal model of brain inflammation. It is an inflammatory demyelinating disease of the central nervous system (CNS). It is mostly used with rodents and is widely studied as an animal model of the human CNS demyelinating diseases, including multiple sclerosis (MS) and acute disseminated encephalomyelitis (ADEM). EAE is also the prototype for T-cell-mediated autoimmune disease in general.

Intrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. It may be due to a variety of reasons such as prolapse or occlusion of the umbilical cord, placental infarction, maternal diabetes and maternal smoking. Intrauterine growth restriction may cause or be the result of hypoxia. Intrauterine hypoxia can cause cellular damage that occurs within the central nervous system. This results in an increased mortality rate, including an increased risk of sudden infant death syndrome (SIDS). Oxygen deprivation in the fetus and neonate have been implicated as either a primary or as a contributing risk factor in numerous neurological and neuropsychiatric disorders such as epilepsy, attention deficit hyperactivity disorder, eating disorders and cerebral palsy.
Brain ischemia is a condition in which there is insufficient bloodflow to the brain to meet metabolic demand. This leads to poor oxygen supply or cerebral hypoxia and thus leads to the death of brain tissue or cerebral infarction/ischemic stroke. It is a sub-type of stroke along with subarachnoid hemorrhage and intracerebral hemorrhage.
Toxic leukoencephalopathy is a rare condition that is characterized by progressive damage (-pathy) to white matter (-leuko-) in the brain (-encephalo-), particularly myelin, due to causes such as exposure to substance use, environmental toxins, or chemotherapeutic drugs. The prevalence of this disease is infrequent and often goes unreported, especially in cases resulting from substance use. Magnetic resonance imaging (MRI) is a popular method to study and diagnose the disease. However, even with technological advances, the exact mechanism and underlying pathophysiology of toxic leukoencephalopathy remains unknown and is thought to vary between sources of toxicity. The clinical severity of toxic leukoencephalopathy also varies among patients, exposure time, concentration, and purity of the toxic agent. Some reversibility of the condition has been seen in many cases when the toxic agent is removed.

Baló's concentric sclerosis is a disease in which the white matter of the brain appears damaged in concentric layers, leaving the axis cylinder intact. It was described by József Mátyás Baló who initially named it "leuko-encephalitis periaxialis concentrica" from the previous definition, and it is currently considered one of the borderline forms of multiple sclerosis.

Leukoencephalopathy with vanishing white matter is an autosomal recessive neurological disease. The cause of the disease are mutations in any of the 5 genes encoding subunits of the translation initiation factor eIF2B: EIF2B1, EIF2B2, EIF2B3, EIF2B4, or EIF2B5. The disease belongs to a family of conditions called the Leukodystrophies.
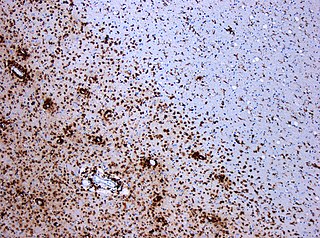
Leukoencephalopathy with neuroaxonal spheroids (LENAS) is an extremely rare kind of leukoencephalopathy and is classified as a neurodegenerative disease. LENAS is a cause of severe and subacute dementia that results from damage to certain areas of the brain. This damage is to a type of brain tissue called white matter and axon damage due to swellings which are termed spheroids.
Neurovirology is an interdisciplinary field which represents a melding of clinical neuroscience, virology, immunology, and molecular biology. The main focus of the field is to study viruses capable of infecting the nervous system. In addition to this, the field studies the use of viruses to trace neuroanatomical pathways, for gene therapy, and to eliminate detrimental populations of neural cells.

Athetoid cerebral palsy, or dyskinetic cerebral palsy, is a type of cerebral palsy primarily associated with damage, like other forms of CP, to the basal ganglia in the form of lesions that occur during brain development due to bilirubin encephalopathy and hypoxic–ischemic brain injury. Unlike spastic or ataxic cerebral palsies, ADCP is characterized by both hypertonia and hypotonia, due to the affected individual's inability to control muscle tone. Clinical diagnosis of ADCP typically occurs within 18 months of birth and is primarily based upon motor function and neuroimaging techniques. While there are no cures for ADCP, some drug therapies as well as speech, occupational therapy, and physical therapy have shown capacity for treating the symptoms.

Hereditary diffuse leukoencephalopathy with spheroids (HDLS) is a rare adult onset autosomal dominant disorder characterized by cerebral white matter degeneration with demyelination and axonal spheroids leading to progressive cognitive and motor dysfunction. Spheroids are axonal swellings with discontinuous or absence of myelin sheaths. It is believed that the disease arises from primary microglial dysfunction that leads to secondary disruption of axonal integrity, neuroaxonal damage, and focal axonal spheroids leading to demyelination. Spheroids in HDLS resemble to some extent those produced by shear stress in a closed head injury with damage to axons, causing them to swell due to blockage of axoplasmic transport. In addition to trauma, axonal spheroids can be found in aged brain, stroke, and in other degenerative diseases. In HDLS, it is uncertain whether demyelination occurs prior to the axonal spheroids or what triggers neurodegeneration after apparently normal brain and white matter development, although genetic deficits suggest that demyelination and axonal pathology may be secondary to microglial dysfunction. The clinical syndrome in patients with HDLS is not specific and it can be mistaken for Alzheimer's disease, frontotemporal dementia, atypical Parkinsonism, multiple sclerosis, or corticobasal degeneration.

Ulegyria is a diagnosis used to describe a specific type of cortical scarring in the deep regions of the sulcus that leads to distortion of the gyri. Ulegyria is identified by its characteristic "mushroom-shaped" gyri, in which scarring causes shrinkage and atrophy in the deep sulcal regions while the surface gyri are spared. This condition is most often caused by hypoxic-ischemic brain injury in the perinatal period. The effects of ulegyria can range in severity, although it is most commonly associated with cerebral palsy, mental retardation and epilepsy. N.C. Bresler was the first to view ulegyria in 1899 and described this abnormal morphology in the brain as “mushroom-gyri." Although ulegyria was first identified in 1899, there is still limited information known or reported about the condition.

Cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL) is disease of the arteries in the brain, which causes tissue loss in the subcortical region of the brain and the destruction of myelin in the CNS. CARASIL is characterized by symptoms such as gait disturbances, hair loss, low back pain, dementia, and stroke. CARASIL is a rare disease, having only been diagnosed in about 50 patients, of which ten have been genetically confirmed. Most cases have been reported in Japan, but Chinese and caucasian individuals have also been diagnosed with the disease. CARASIL is inherited in an autosomal recessive pattern. There is currently no cure for CARASIL. Other names for CARASIL include familial young-adult-onset arteriosclerotic leukoencephalopathy with alopecia and lumbago without arterial hypertension, Nemoto disease and Maeda syndrome.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Schprecher, David; Mehta, Lahar (January 2010). "The syndrome of delayed post-hypoxic leukoencephalopathy". NeuroRehabilitation. 26 (1): 65–72. doi:10.3233/NRE-2010-0536. PMC 2835522 . PMID 20166270.
- 1 2 3 Pantoni MD, Leonardo; Garcia MD; Julio H (1997). "Pathogenesis of Leukoaraiosis". Stroke. 28 (3): 652–659. doi:10.1161/01.STR.28.3.652. hdl: 2434/579412 . PMID 9056627.
- 1 2 3 4 Custodio, Christian M; Basford, Jeffrey R (March 2004). "Delayed postanoxic encephalopathy: a case report and literature review". Archives of Physical Medicine and Rehabilitation. 85 (3): 502–505. doi:10.1016/S0003-9993(03)00471-4. PMID 15031841.
- ↑ H. Bour, Iain McAllan Ledingham, Iain McA. Ledingham (1967) Carbon Monoxide Poisoning. p.73
- ↑ Hideo H. Itabashi, MD, John M. Andrews, MD, Uwamie Tomiyasu, MD (2007) Forensic Neuropathology: A Practical Review of the Fundamentals. p.295
- 1 2 PLUM, FRED (July 1962). "Delayed Neurological Deterioration After Anoxia". Archives of Internal Medicine. 110 (1): 18–25. doi:10.1001/archinte.1962.03620190020003. PMID 14487254.
- ↑ Okeda R, Song S.-Y., Funta N, Higashino F (1983). "An experimental study of the pathogenesis of Grinker's myelinopathy in carbon monoxide intoxication". Acta Neuropathologica. 59 (3): 200–2006. doi:10.1007/BF00703204. PMID 6845982.
- ↑ Sprecher, David; Flanigan, K.; Smith, G.A.; Smith, S.; Schenkenberg, T.; Steffens, J. (September 2008). "Clinical and Diagnostic Features of Delayed Hypoxic Leukoencephalopathy". The Journal of Neuropsychiatry and Clinical Neurosciences. 20 (4).