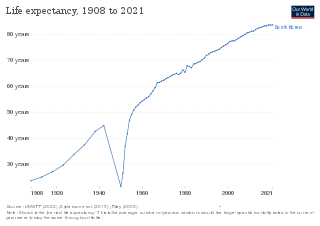
Human life expectancy is a statistical measure of the estimate of the average remaining years of life at a given age. The most commonly used measure is life expectancy at birth. This can be defined in two ways. Cohort LEB is the mean length of life of a birth cohort and can be computed only for cohorts born so long ago that all their members have died. Period LEB is the mean length of life of a hypothetical cohort assumed to be exposed, from birth through death, to the mortality rates observed at a given year. National LEB figures reported by national agencies and international organizations for human populations are estimates of period LEB.
Lifestyle diseases can be defined as diseases linked with one's lifestyle. These diseases are non-communicable diseases. They are caused by lack of physical activity, unhealthy eating, alcohol, substance use disorders and smoking tobacco, which can lead to heart disease, stroke, obesity, type II diabetes and lung cancer. The diseases that appear to increase in frequency as countries become more industrialized and people live longer include Alzheimer's disease, arthritis, atherosclerosis, asthma, cancer, chronic liver disease or cirrhosis, chronic obstructive pulmonary disease, colitis, irritable bowel syndrome, type 2 diabetes, heart disease, hypertension, metabolic syndrome, chronic kidney failure, osteoporosis, PCOD, stroke, depression, obesity and vascular dementia.

Preventive healthcare, or prophylaxis, is the application of healthcare measures to prevent diseases. Disease and disability are affected by environmental factors, genetic predisposition, disease agents, and lifestyle choices, and are dynamic processes that begin before individuals realize they are affected. Disease prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention.

Diseases of affluence, previously called diseases of rich people, is a term sometimes given to selected diseases and other health conditions which are commonly thought to be a result of increasing wealth in a society. Also referred to as the "Western disease" paradigm, these diseases are in contrast to so-called "diseases of poverty", which largely result from and contribute to human impoverishment. These diseases of affluence have vastly increased in prevalence since the end of World War II.
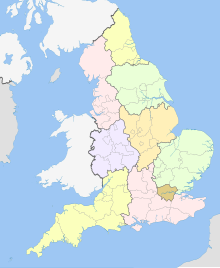
Health in the United Kingdom refers to the overall health of the population of the United Kingdom. This includes overall trends such as life expectancy and mortality rates, mental health of the population and the suicide rate, smoking rates, alcohol consumption, prevalence of diseases within the population and obesity in the United Kingdom. Three of these – smoking rates, alcohol consumption and obesity – were above the OECD average in 2015.
Australia is a high income country, and this is reflected in the good status of health of the population overall. In 2011, Australia ranked 2nd on the United Nations Development Programme's Human Development Index, indicating the level of development of a country. Despite the overall good status of health, the disparities occurring in the Australian healthcare system are a problem. The poor and those living in remote areas as well as indigenous people are, in general, less healthy than others in the population, and programs have been implemented to decrease this gap. These include increased outreach to the indigenous communities and government subsidies to provide services for people in remote or rural areas.
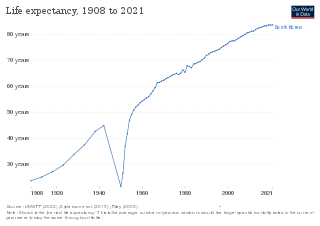
Life expectancy has been rising rapidly and South Korea ranked 3rd in the world for life expectancy. South Korea has among the lowest HIV/AIDS adult prevalence rate in the world, with just 0.1% of the population being infected, significantly lower than the U.S. at 0.6%, France's 0.4%, and the UK's 0.3% prevalence rate. South Korea has a good influenza vaccination rate, with a total of 43.5% of the population being vaccinated in 2019. A new measure of expected human capital calculated for 195 countries from 1920 to 2016 and defined for each birth cohort as the expected years lived from age 20 to 64 years and adjusted for educational attainment, learning or education quality, and functional health status was published by the Lancet in September 2018. South Korea had the sixth highest level of expected human capital with 26 health, education, and learning-adjusted expected years lived between age 20 and 64 years.
Social epidemiology focuses on the patterns in morbidity and mortality rates that emerge as a result of social characteristics. While an individual's lifestyle choices or family history may place him or her at an increased risk for developing certain illnesses, there are social inequalities in health that cannot be explained by individual factors. Variations in health outcomes in the United States are attributed to several social characteristics, such as gender, race, socioeconomic status, the environment, and educational attainment. Inequalities in any or all of these social categories can contribute to health disparities, with some groups placed at an increased risk for acquiring chronic diseases than others.
Chronic, non-communicable diseases account for an estimated 80% of total deaths and 70% of disability-adjusted life years (DALYs) lost in China. Cardiovascular diseases, chronic respiratory disease, and cancer are the leading causes of both death and of the burden of disease, and exposure to risk factors is high: more than 300 million men smoke cigarettes and 160 million adults are hypertensive, most of whom are not being treated. An obesity epidemic is imminent, with more than 20% of children aged 7–17 years in big cities now overweight or obese. Rates of death from chronic disease in middle-aged people are higher in China than in some high-income countries.

The healthcare system in Turkey has improved in terms of health status especially after implementing the Health Transformation Program (HP) in 2003. "Health for All" was the slogan for this transformation, and HP aimed to provide and finance health care efficiently, effectively, and equitably. By covering most of the population, the General Health Insurance Scheme is financed by employers, employees, and government contributions through the Social Security Institution. Even though HP aimed to be equitable, after 18 years of implementation, there are still disparities between the regions in Turkey. While the under-5 mortality rate in Western Marmara is 7.9, the under-5 mortality rate in Southeastern Asia is two times higher than Western Marmara, with the rate of 16.3 in 2021.

The major causes of deaths in Finland are cardiovascular diseases, malignant tumors, dementia and Alzheimer's disease, respiratory diseases, alcohol related diseases and accidental poisoning by alcohol. In 2010, the leading causes of death among men aged 15 to 64 were alcohol related deaths, ischaemic heart disease, accident, suicides, lung cancer and cerebrovascular diseases. Among women the leading causes were breast cancer, alcohol related deaths, accidents, suicides, ischaemic heart disease and lung cancer.
Health in Wales refers to the overall health of the population of Wales.

Italy is known for its generally very good health system, and the life expectancy is 80 for males and 85 for females, placing the country 5th in the world for life expectancy, and low infant mortality. In comparison to other Western countries, Italy has a relatively low rate of adult obesity, as there are several health benefits of the Mediterranean diet. The proportion of daily smokers was 22% in 2012, down from 24.4% in 2000 but still slightly above the OECD average. Smoking in public places including bars, restaurants, night clubs and offices has been restricted to specially ventilated rooms since 2005.
In 2006, life expectancy for males in Cyprus was 79 and for females 82 years. Infant mortality in 2002 was 5 per 1,000 live births, comparing favourably to most developed nations.

The Glasgow effect is an outdated term which referred to the lower life expectancy of residents of Glasgow compared to the rest of the United Kingdom and Europe. The phenomenon is defined as an "[e]xcess mortality in the West of Scotland (Glasgow) after controlling for deprivation." Although lower income levels are generally associated with poor health and a shorter lifespan, epidemiologists have argued that poverty alone does not appear to account for the disparity found in Glasgow. Equally deprived areas of the UK such as Liverpool and Manchester have higher life expectancies, and the wealthiest ten percent of the Glasgow population have a lower life expectancy than the same group in other cities. One in four men in Glasgow will die before his sixty-fifth birthday.
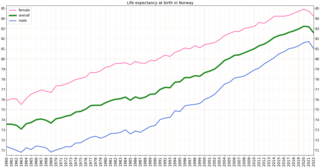
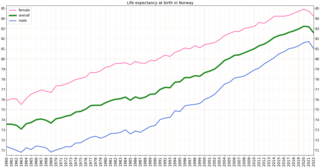
Health in Norway, with its early history of poverty and infectious diseases along with famines and epidemics, was poor for most of the population at least into the 1800s. The country eventually changed from a peasant society to an industrial one and established a public health system in 1860. Due to the high life expectancy at birth, the low under five mortality rate and the fertility rate in Norway, it is fair to say that the overall health status in the country is generally good.
Males make up just under half of the total Australian population of 23 million. On average Australian males live to around 78 years of age, with the life expectancy of an Indigenous Australian male in 2009 being around 67 years of age and non indigenous men in remote areas living to around 70. On average female mortality rates are lower than males across the entire age spectrum.
Montenegro is a country with an area of 13,812 square kilometres and a population of 620,029, according to the 2011 census. The country is bordered by Croatia, the Adriatic Sea, Bosnia, Herzegovina, Serbia, Kosovo and Albania. The most common health issues faced are non-communicable diseases accounting for 95% of all deaths. This is followed by 4% of mortality due to injury, and 1% due to communicable, maternal, perinatal and nutritional conditions. Other health areas of interest are alcohol consumption, which is the most prevalent disease of addiction within Montenegro and smoking. Montenegro has one of the highest tobacco usage rates across Europe. Life expectancy for men is 74 years, and life expectancy for women is 79.