A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.

Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. It includes work done in providing primary care, secondary care, and tertiary care, as well as in public health.

Publicly funded healthcare is a form of health care financing designed to meet the cost of all or most healthcare needs from a publicly managed fund. Usually this is under some form of democratic accountability, the right of access to which are set down in rules applying to the whole population contributing to the fund or receiving benefits from it.

The healthcare industry is an aggregation and integration of sectors within the economic system that provides goods and services to treat patients with curative, preventive, rehabilitative, and palliative care. It includes the generation and commercialization of goods and services lending themselves to maintaining and re-establishing health. The modern healthcare industry includes three essential branches which are services, products, and finance, and may be divided into many sectors and categories and depends on the interdisciplinary teams of trained professionals and paraprofessionals to meet the health needs of individuals and populations.

Healthcare in Canada is delivered through the provincial and territorial systems of publicly funded health care, informally called Medicare. It is guided by the provisions of the Canada Health Act of 1984, and is universal. The 2002 Royal Commission, known as the Romanow Report, revealed that Canadians consider universal access to publicly funded health services as a "fundamental value that ensures national health care insurance for everyone wherever they live in the country."

Two-tier healthcare is a situation in which a basic government-provided healthcare system provides basic care, and a secondary tier of care exists for those who can pay for additional, better quality or faster access. Most countries have both publicly and privately funded healthcare, but the degree to which it creates a quality differential depends on the way the two systems are managed, funded, and regulated.

The health care system in Japan provides different types of services, including screening examinations, prenatal care and infectious disease control, with the patient accepting responsibility for 30% of these costs while the government pays the remaining 70%. Payment for personal medical services is offered by a universal health care insurance system that provides relative equality of access, with fees set by a government committee. All residents of Japan are required by the law to have health insurance coverage. People without insurance from employers can participate in a national health insurance program, administered by local governments. Patients are free to select physicians or facilities of their choice and cannot be denied coverage. Hospitals, by law, must be run as non-profit and be managed by physicians.
A public hospital, or government hospital, is a hospital which is government owned and is fully funded by the government and operates solely off the money that is collected from taxpayers to fund healthcare initiatives. In some countries, this type of hospital provides medical care free of charge to patients, covering expenses and wages by government reimbursement.

The Swedish health care system is mainly government-funded, universal for all citizens and decentralized, although private health care also exists. The health care system in Sweden is financed primarily through taxes levied by county councils and municipalities. A total of 21 councils are in charge with primary and hospital care within the country.

Healthcare in South Korea is universal, although a significant portion of healthcare is privately funded. South Korea's healthcare system is based on the National Health Insurance Service, a public health insurance program run by the Ministry of Health and Welfare to which South Koreans of sufficient income must pay contributions in order to insure themselves and their dependants, and the Medical Aid Program, a social welfare program run by the central government and local governments to insure those unable to pay National Health Insurance contributions. In 2015, South Korea ranked first in the OECD for healthcare access. Satisfaction of healthcare has been consistently among the highest in the world – South Korea was rated as the second most efficient healthcare system by Bloomberg. Health insurance in South Korea is single-payer system. The introduction of health insurance resulted in a significant surge in the utilization of healthcare services. Healthcare providers are overburdened by low reimbursement rates.
Healthcare in Finland consists of a highly decentralized three-level publicly funded healthcare system and a much smaller private sector. Although the Ministry of Social Affairs and Health has the highest decision-making authority, specific healthcare precincts are responsible for providing healthcare to their residents as of 2023.
Kenya's health care system is structured in a step-wise manner so that complicated cases are referred to a higher level. Gaps in the system are filled by private and church run units.

Hungary has a tax-funded universal healthcare system, organized by the state-owned National Health Insurance Fund. While healthcare is considered universal, several reasons persist preventing Hungarian nationals to access healthcare services. For instance, a Hungarian citizen who lived abroad but is unable to show contributions to another country's healthcare system will not be able to access the Hungarian healthcare system free of charge. However, to the OECD, 100% of the total population is covered by universal health insurance, which is absolutely free for children, mothers or fathers with babies, students, pensioners, people with low income, handicapped people, priests and other church employees. In 2022 the cost of public health insurance is 8,400 HUF per month which is the equivalent of $23.69. The healthcare system underwent significant changes which also resulted in improving life expectancy and a very low infant mortality rate. According to the OECD Hungary spent 7.8% of its GDP on health care in 2012. Total health expenditure was $US1,688.7 per capita in 2011, US$1,098.3governmental-fund (65%) and US$590.4 private-fund (35%).

Healthcare in Slovenia is organised primarily through the Health Insurance Institute of Slovenia. In 2015, healthcare expenditures accounted for 8.10% of GDP. The Slovenian healthcare system was ranked 15th in the Euro health consumer index 2015. The country ranked second in the 2012 Euro Hepatitis Index.
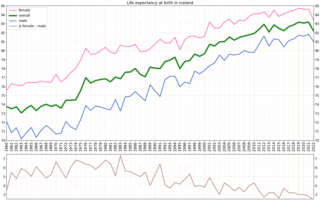
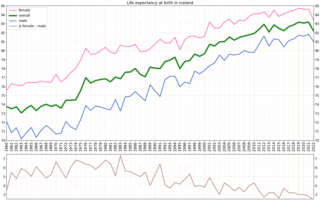
Iceland has a state-centred, publicly funded universal healthcare system and health insurance that covers the whole population. The number of private providers in Iceland has increased. The healthcare system is largely paid for by taxes (84%) and to some extent by service fees (16%) and is administrated by the Ministry of Health. A considerable portion of government spending is assigned to healthcare. There is almost no private health insurance in Iceland and no private hospitals. In very limited cases, access to a private provider can be reimbursement for services provided that the conditions are met.

Healthcare in Greece consists of a universal health care system provided through national health insurance, and private health care. According to the 2011 budget, the Greek healthcare system was allocated 6.1 billion euro, or 2.8% of GDP. In a 2000 report by the World Health Organization, the Greek healthcare system was ranked 14th worldwide in the overall assessment, above other countries such as Germany (25) and the United Kingdom (18), while ranking 11th at level of service.
Examples of health care systems of the world, sorted by continent, are as follows.

As of 2019 Lithuanian life expectancy at birth was 76.0 and the infant mortality rate was 2.99 per 1,000 births. This is below the EU and OECD average.
Health care finance in the United States discusses how Americans obtain and pay for their healthcare, and why U.S. healthcare costs are the highest in the world based on various measures.