Related Research Articles

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.
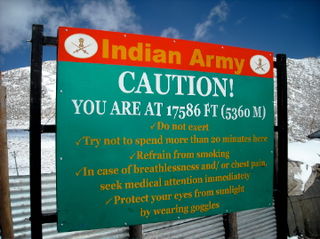
Altitude sickness, the mildest form being acute mountain sickness (AMS), is the harmful effect of high altitude, caused by rapid exposure to low amounts of oxygen at high elevation. People can respond to high altitude in different ways. Symptoms may include headaches, vomiting, tiredness, confusion, trouble sleeping, and dizziness. Acute mountain sickness can progress to high-altitude pulmonary edema (HAPE) with associated shortness of breath or high-altitude cerebral edema (HACE) with associated confusion. Chronic mountain sickness may occur after long-term exposure to high altitude.

Papilledema or papilloedema is optic disc swelling that is caused by increased intracranial pressure due to any cause. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare.

Dexamethasone is a glucocorticoid medication used to treat rheumatic problems, a number of skin diseases, severe allergies, asthma, chronic obstructive lung disease, croup, brain swelling, eye pain following eye surgery, superior vena cava syndrome, and along with antibiotics in tuberculosis. In adrenocortical insufficiency, it may be used in combination with a mineralocorticoid medication such as fludrocortisone. In preterm labor, it may be used to improve outcomes in the baby. It may be given by mouth, as an injection into a muscle, as an injection into a vein, as a topical cream or ointment for the skin or as a topical ophthalmic solution to the eye. The effects of dexamethasone are frequently seen within a day and last for about three days.

Acetazolamide, sold under the trade name Diamox among others, is a medication used to treat glaucoma, epilepsy, altitude sickness, periodic paralysis, idiopathic intracranial hypertension, heart failure and to alkalinize urine. It may be used long term for the treatment of open angle glaucoma and short term for acute angle closure glaucoma until surgery can be carried out. It is taken by mouth or injection into a vein. Acetazolamide is a first generation carbonic anhydrase inhibitor and it decreases the ocular fluid and osmolality in the eye to decrease intraocular pressure.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, coma and death.

Pulmonary edema, also known as pulmonary congestion, is excessive liquid accumulation in the tissue and air spaces of the lungs. It leads to impaired gas exchange and may cause hypoxemia and respiratory failure. It is due to either failure of the left ventricle of the heart to remove oxygenated blood adequately from the pulmonary circulation, or an injury to the lung tissue directly or blood vessels of the lung.
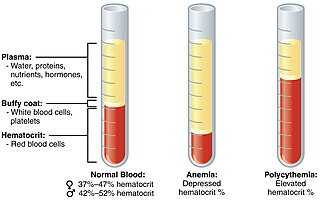
Polycythemia is a laboratory finding in which the hematocrit and/or hemoglobin concentration are increased in the blood. Polycythemia is sometimes called erythrocytosis, and there is significant overlap in the two findings, but the terms are not the same: polycythemia describes any increase in hematocrit and/or hemoglobin, while erythrocytosis describes an increase specifically in the number of red blood cells in the blood.
In mountaineering, the death zone refers to altitudes above a certain point where the pressure of oxygen is insufficient to sustain human life for an extended time span. This point is generally tagged as 8,000 m. The concept was conceived in 1953 by Edouard Wyss-Dunant, a Swiss doctor, who called it the lethal zone. All 14 peaks above 8000 m in the death zone are located in the Himalaya and Karakoram of Asia.

Generalized hypoxia is a medical condition in which the tissues of the body are deprived of the necessary levels of oxygen due to an insufficient supply of oxygen, which may be due to the composition or pressure of the breathing gas, decreased lung ventilation, or respiratory disease, any of which may cause a lower than normal oxygen content in the arterial blood, and consequently a reduced supply of oxygen to all tissues perfused by the arterial blood. This usage is in contradistinction to localized hypoxia, in which only an associated group of tissues, usually with a common blood supply, are affected, usually due to an insufficient or reduced blood supply to those tissues. Generalized hypoxia is also used as a synonym for hypoxic hypoxia This is not to be confused with hypoxemia, which refers to low levels of oxygen in the blood, although the two conditions often occur simultaneously, since a decrease in blood oxygen typically corresponds to a decrease in oxygen in the surrounding tissue. However, hypoxia may be present without hypoxemia, and vice versa, as in the case of infarction. Several other classes of medical hypoxia exist.

High-altitude pulmonary edema (HAPE) is a life-threatening form of non-cardiogenic pulmonary edema that occurs in otherwise healthy people at altitudes typically above 2,500 meters (8,200 ft). However, cases have also been reported between 1,500–2,500 metres or 4,900–8,200 feet in more vulnerable subjects.
Stridor is a high-pitched extra-thoracic breath sound resulting from turbulent air flow in the larynx or lower in the bronchial tree. It is different from a stertor which is a noise originating in the pharynx. Stridor is a physical sign which is caused by a narrowed or obstructed airway. It can be inspiratory, expiratory or biphasic, although it is usually heard during inspiration. Inspiratory stridor often occurs in children with croup. It may be indicative of serious airway obstruction from severe conditions such as epiglottitis, a foreign body lodged in the airway, or a laryngeal tumor. Stridor should always command attention to establish its cause. Visualization of the airway by medical experts equipped to control the airway may be needed.

Cerebral hypoxia is a form of hypoxia, specifically involving the brain; when the brain is completely deprived of oxygen, it is called cerebral anoxia. There are four categories of cerebral hypoxia; they are, in order of increasing severity: diffuse cerebral hypoxia (DCH), focal cerebral ischemia, cerebral infarction, and global cerebral ischemia. Prolonged hypoxia induces neuronal cell death via apoptosis, resulting in a hypoxic brain injury.
Hypoxic pulmonary vasoconstriction (HPV), also known as the Euler-Liljestrand mechanism, is a physiological phenomenon in which small pulmonary arteries constrict in the presence of alveolar hypoxia. By redirecting blood flow from poorly-ventilated lung regions to well-ventilated lung regions, HPV is thought to be the primary mechanism underlying ventilation/perfusion matching.
Chronic mountain sickness (CMS) is a disease in which the proportion of blood volume that is occupied by red blood cells increases (polycythaemia) and there is an abnormally low level of oxygen in the blood (hypoxemia). CMS typically develops after extended time living at high altitude. It is most common amongst native populations of high altitude nations. The most frequent symptoms of CMS are headache, dizziness, tinnitus, breathlessness, palpitations, sleep disturbance, fatigue, loss of appetite, confusion, cyanosis, and dilation of veins.

Carbonic anhydrase inhibitors are a class of pharmaceuticals that suppress the activity of carbonic anhydrase. Their clinical use has been established as anti-glaucoma agents, diuretics, antiepileptics, in the management of mountain sickness, gastric and duodenal ulcers, idiopathic intracranial hypertension, neurological disorders, or osteoporosis.

Posterior reversible encephalopathy syndrome (PRES), also known as reversible posterior leukoencephalopathy syndrome (RPLS), is a rare condition in which parts of the brain are affected by swelling, usually as a result of an underlying cause. Someone with PRES may experience headache, changes in vision, and seizures, with some developing other neurological symptoms such as confusion or weakness of one or more limbs. The name of the condition includes the word "posterior" because it predominantly though not exclusively affects the back of the brain. Common underlying causes are severely elevated blood pressure, kidney failure, severe infections, certain medications, some autoimmune diseases, and pre-eclampsia. The diagnosis is usually made by brain scan (MRI) on which areas of swelling can be identified.

The effects of high altitude on humans are mostly the consequences of reduced partial pressure of oxygen in the atmosphere. The oxygen saturation of hemoglobin determines the content of oxygen in blood. After the human body reaches around 2,100 metres (6,900 ft) above sea level, the saturation of oxyhemoglobin begins to decrease rapidly. However, the human body has both short-term and long-term adaptations to altitude that allow it to partially compensate for the lack of oxygen. There is a limit to the level of adaptation; mountaineers refer to the altitudes above 8,000 metres (26,000 ft) as the death zone, where it is generally believed that no human body can acclimatize. At extreme altitudes, the ambient pressure can drop below the vapor pressure of water at body temperature, but at such altitudes even pure oxygen at ambient pressure cannot support human life, and a pressure suit is necessary. A rapid depressurisation to the low pressures of high altitudes can trigger altitude decompression sickness.
Grinker's myelinopathy, also known as anoxic leukoencephalopathy, is a rare disease of the central nervous system. The disease is characterized by a delayed leukoencephalopathy after a hypoxic episode. It is typically, though not necessarily, related to carbon monoxide poisoning or heroin overdose. It occurs in roughly 2.8% of those who experience an acute hypoxic/anoxic episode. Because of the wide range of symptoms and the delay in onset, it is often misdiagnosed as other neuropathologies. Grinker's myelinopathy was originally characterized by Roy R. Grinker in 1925 or 1926, depending on the source.

Silent hypoxia is generalised hypoxia that does not coincide with shortness of breath. This presentation is known to be a complication of COVID-19, and is also known in walking pneumonia, altitude sickness, and rebreather diving.
References
- ↑ 'Oedema' is the standard form defined in the Concise Oxford English Dictionary (2011), with the precision that the spelling in the United States is 'edema'.
- 1 2 3 Bärtsch & Swenson 2013, p. 2296.
- 1 2 3 Rosenberg 2012, p. 146.
- 1 2 3 4 5 Bärtsch & Swenson 2013, p. 2294.
- 1 2 3 4 5 6 7 8 9 10 Schoene et al. 2012, p. 301.
- ↑ Wilson, Newman & Imray 2009, p. 185.
- 1 2 3 Wilson, Newman & Imray 2009, p. 177.
- 1 2 3 4 5 Schoene et al. 2012, p. 303.
- 1 2 3 4 5 6 7 8 9 Schoene et al. 2012, p. 304.
- ↑ Imray et al. 2010, p. 470.
- ↑ Imray et al. 2010, p. 468.
- ↑ Imray et al. 2010, p. 469.
- 1 2 3 4 Rosenberg 2012, p. 147.
- ↑ Wilson, Newman & Imray 2009, p. 182.
- ↑ Rosenberg 2012, pp. 146–50.
- 1 2 3 4 5 6 7 8 Bärtsch & Swenson 2013, p. 2295.
- 1 2 3 4 5 Schoene et al. 2012, p. 306.
- 1 2 3 4 Rosenberg 2012, p. 148.
- 1 2 3 Schoene et al. 2012, p. 305.
- 1 2 3 4 5 6 7 8 Schoene 2008.
- ↑ Wilson, Newman & Imray 2009, p. 183.
- 1 2 Wilson, Newman & Imray 2009, p. 181.
- ↑ Imray et al. 2010, p. 474.
- ↑ Imray et al. 2010, p. 472.
- 1 2 3 Schoene et al. 2012, p. 307.
- 1 2 Imray et al. 2010, p. 467.
- 1 2 3 Wilson, Newman & Imray 2009, p. 175.
- ↑ Bärtsch & Swenson 2013, p. 2298.
- 1 2 Imray et al. 2010, p. 471.
- 1 2 Bärtsch & Swenson 2013, p. 2299.
- ↑ Luks, Andrew; Scott E. Macintosh; Colin K. Grissom; Paul S Auerbach; George W Rodway; Robert B Schoene; Ken Zafren; Peter H Hackett (June 2010). "Wilderness Medical Society Consensus Guidelines for the Prevention and Treatment of Acute Altitude Illness". Wilderness & Environmental Medicine. 21 (2): 146–155. doi: 10.1016/j.wem.2010.03.002 . PMID 20591379 . Retrieved 13 December 2013.
- ↑ Luks, Andrew; Scott E. Macintosh; Colin K. Grissom; Paul S Auerbach; George W Rodway; Robert B Schoene; Ken Zafren; Peter H Hackett (June 2010). "Wilderness Medical Society Consensus Guidelines for the Prevention and Treatment of Acute Altitude Illness". Wilderness & Environmental Medicine. 21 (2): 146–155. doi: 10.1016/j.wem.2010.03.002 . PMID 20591379 . Retrieved 13 December 2013.
- ↑ Wilson, Newman & Imray 2009, p. 179.
- 1 2 Imray et al. 2010, p. 478.
- ↑ Wilson, Newman & Imray 2009, p. 176.
- ↑ Rosenberg 2012, pp. 146 & 150.
- ↑ Wilson, Newman & Imray 2009, p. 184.
- ↑ Bärtsch & Swenson 2013, p. 2300.
- ↑ Imray et al. 2010, p. 475.
- ↑ Wilson, Newman & Imray 2009, p. 180.