Cartilage is a resilient and smooth type of connective tissue. In tetrapods, it covers and protects the ends of long bones at the joints as articular cartilage, and is a structural component of many body parts including the rib cage, the neck and the bronchial tubes, and the intervertebral discs. In other taxa, such as chondrichthyans, but also in cyclostomes, it may constitute a much greater proportion of the skeleton. It is not as hard and rigid as bone, but it is much stiffer and much less flexible than muscle. The matrix of cartilage is made up of glycosaminoglycans, proteoglycans, collagen fibers and, sometimes, elastin.
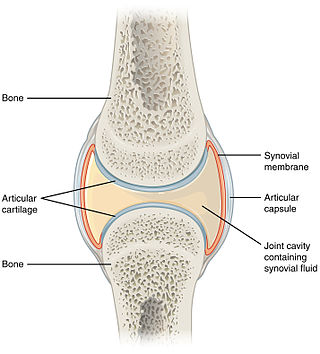
The synovial membrane is a specialized connective tissue that lines the inner surface of capsules of synovial joints and tendon sheath. It makes direct contact with the fibrous membrane on the outside surface and with the synovial fluid lubricant on the inside surface. In contact with the synovial fluid at the tissue surface are many rounded macrophage-like synovial cells and also type B cells, which are also known as fibroblast-like synoviocytes (FLS). Type A cells maintain the synovial fluid by removing wear-and-tear debris. As for the FLS, they produce hyaluronan, as well as other extracellular components in the synovial fluid.
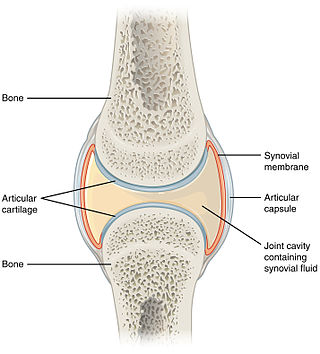
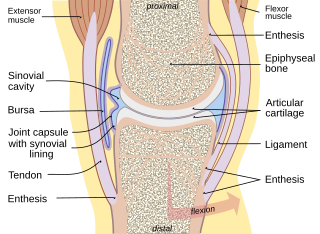
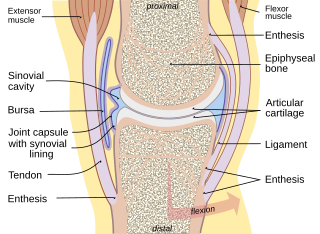
A synovial joint, also known as diarthrosis, joins bones or cartilage with a fibrous joint capsule that is continuous with the periosteum of the joined bones, constitutes the outer boundary of a synovial cavity, and surrounds the bones' articulating surfaces. This joint unites long bones and permits free bone movement and greater mobility. The synovial cavity/joint is filled with synovial fluid. The joint capsule is made up of an outer layer of fibrous membrane, which keeps the bones together structurally, and an inner layer, the synovial membrane, which seals in the synovial fluid.

The periosteum is a membrane that covers the outer surface of all bones, except at the articular surfaces of long bones. Endosteum lines the inner surface of the medullary cavity of all long bones.
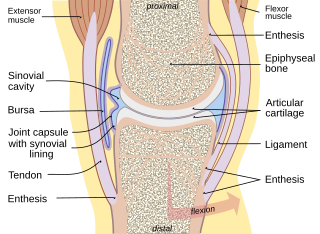
Synovial fluid, also called synovia,[help 1] is a viscous, non-Newtonian fluid found in the cavities of synovial joints. With its egg white–like consistency, the principal role of synovial fluid is to reduce friction between the articular cartilage of synovial joints during movement. Synovial fluid is a small component of the transcellular fluid component of extracellular fluid.

Chondrocytes are the only cells found in healthy cartilage. They produce and maintain the cartilaginous matrix, which consists mainly of collagen and proteoglycans. Although the word chondroblast is commonly used to describe an immature chondrocyte, the term is imprecise, since the progenitor of chondrocytes can differentiate into various cell types, including osteoblasts.

Chondroblasts, or perichondrial cells, is the name given to mesenchymal progenitor cells in situ which, from endochondral ossification, will form chondrocytes in the growing cartilage matrix. Another name for them is subchondral cortico-spongious progenitors. They have euchromatic nuclei and stain by basic dyes.

Chondrogenesis is the process by which cartilage is developed.
Articular cartilage, most notably that which is found in the knee joint, is generally characterized by very low friction, high wear resistance, and poor regenerative qualities. It is responsible for much of the compressive resistance and load bearing qualities of the knee joint and, without it, walking is painful to impossible. Osteoarthritis is a common condition of cartilage failure that can lead to limited range of motion, bone damage and invariably, pain. Due to a combination of acute stress and chronic fatigue, osteoarthritis directly manifests itself in a wearing away of the articular surface and, in extreme cases, bone can be exposed in the joint. Some additional examples of cartilage failure mechanisms include cellular matrix linkage rupture, chondrocyte protein synthesis inhibition, and chondrocyte apoptosis. There are several different repair options available for cartilage damage or failure.

An isogenous group is a cluster of up to eight chondrocytes found in hyaline and elastic cartilage.

Fibroblast growth factor 18 (FGF18) is a protein that is encoded by the Fgf18 gene in humans. The protein was first discovered in 1998, when two newly-identified murine genes Fgf17 and Fgf18 were described and confirmed as being closely related by sequence homology to Fgf8. The three proteins were eventually grouped into the FGF8 subfamily, which contains several of the endocrine FGF superfamily members FGF8, FGF17, and FGF18. Subsequent studies identified FGF18's role in promoting chondrogenesis, and an apparent specific activity for the generation of the hyaline cartilage in articular joints.

Proteoglycan 4 or lubricin is a proteoglycan that in humans is encoded by the PRG4 gene. It acts as a joint/boundary lubricant.
Articular cartilage repair treatment involves the repair of the surface of an articular joint's hyaline cartilage. Over the last few decades, surgeons and researchers have made progress in elaborating surgical cartilage repair interventions. Though these solutions do not perfectly restore the articular cartilage, some of the latest technologies have started to bring very promising results in repairing cartilages from traumatic injuries or chondropathies. These treatments have been shown to be especially beneficial for patients who have articular cartilage damage. They can provide some measure of pain relief, while at the same time slowing down the accumulation of damage, or considerably delaying the need for joint replacement surgery.
Autologous chondrocyte implantation is a biomedical treatment that repairs damages in articular cartilage. ACI provides pain relief while at the same time slowing down the progression or considerably delaying partial or total joint replacement surgery. The goal of ACI is to allow people suffering from articular cartilage damage to return to their old lifestyle; regaining mobility, going back to work and even practicing sports again.
Mesenchymal stem cells (MSCs) are multipotent cells found in multiple human adult tissues including bone marrow, synovial tissues, and adipose tissues. Since they are derived from the mesoderm, they have been shown to differentiate into bone, cartilage, muscle, and adipose tissue. MSCs from embryonic sources have shown promise scientifically while creating significant controversy. As a result, many researchers have focused on adult stem cells, or stem cells isolated from adult humans that can be transplanted into damaged tissue.
Autologous matrix-induced chondrogenesis (AMIC) is a treatment for articular cartilage damage. It combines microfracture surgery with the application of a bi-layer collagen I/III membrane. There is tentative short to medium term benefits as of 2017.
Gene therapy for osteoarthritis is the application of gene therapy to treat osteoarthritis (OA). Unlike pharmacological treatments which are administered locally or systemically as a series of interventions, gene therapy aims to establish sustained therapeutic effect after a single, local injection.
Sprifermin (INN), is a recombinant human fibroblast growth factor 18 (rhFGF18) analog, which is under development by TrialSpark for the treatment of osteoarthritis. FGF18 and sprifermin act via the Fibroblast Growth Factor Receptor (FGFR) family, with preferential activity via FGFR3c.
Nasal chondrocytes (NC) are present in the hyaline cartilage of the nasal septum and in fact are the only cell type within the tissue. Similar to chondrocytes present in articular cartilage, NC express extracellular matrix proteins such as glycosaminoglycans and collagen.
Artificial cartilage is a synthetic material made of hydrogels or polymers that aims to mimic the functional properties of natural cartilage in the human body. Tissue engineering principles are used in order to create a non-degradable and biocompatible material that can replace cartilage. While creating a useful synthetic cartilage material, certain challenges need to be overcome. First, cartilage is an avascular structure in the body and therefore does not repair itself. This creates issues in regeneration of the tissue. Synthetic cartilage also needs to be stably attached to its underlying surface i.e. the bone. Lastly, in the case of creating synthetic cartilage to be used in joint spaces, high mechanical strength under compression needs to be an intrinsic property of the material.