Related Research Articles
A bronchodilator or broncholytic is a substance that dilates the bronchi and bronchioles, decreasing resistance in the respiratory airway and increasing airflow to the lungs. Bronchodilators may be originating naturally within the body, or they may be medications administered for the treatment of breathing difficulties, usually in the form of inhalers. They are most useful in obstructive lung diseases, of which asthma and chronic obstructive pulmonary disease are the most common conditions. Although this remains somewhat controversial, they might be useful in bronchiolitis and bronchiectasis. They are often prescribed but of unproven significance in restrictive lung diseases.

Ciclosporin, also spelled cyclosporine and cyclosporin, is a calcineurin inhibitor, used as an immunosuppressant medication. It is taken orally or intravenously for rheumatoid arthritis, psoriasis, Crohn's disease, nephrotic syndrome, eczema, and in organ transplants to prevent rejection. It is also used as eye drops for keratoconjunctivitis sicca.

Tacrolimus, sold under the brand name Prograf among others, is an immunosuppressive drug. After allogenic organ transplant, the risk of organ rejection is moderate. To lower the risk of organ rejection, tacrolimus is given. The drug can also be sold as a topical medication in the treatment of T-cell-mediated diseases such as eczema and psoriasis. For example, it is prescribed for severe refractory uveitis after a bone marrow transplant, exacerbations of minimal change disease, Kimura's disease, and vitiligo. It can be used to treat dry eye syndrome in cats and dogs.

Immunosuppressive drugs, also known as immunosuppressive agents, immunosuppressants and antirejection medications, are drugs that inhibit or prevent the activity of the immune system.

A spacer is a device used to increase the ease of administering aerosolized medication from a metered-dose inhaler (MDI). It adds space in the form of a tube or "chamber" between the mouth and canister of medication. Most spacers have a one-way valve that allows the person to inhale the medication while inhaling and exhaling normally; these are often referred to as valved holding chambers (VHC).

Salbutamol, also known as albuterol and sold under the brand name Ventolin among others, is a medication that opens up the medium and large airways in the lungs. It is a short-acting β2 adrenergic receptor agonist which works by causing relaxation of airway smooth muscle. It is used to treat asthma, including asthma attacks and exercise-induced bronchoconstriction, as well as chronic obstructive pulmonary disease (COPD). It may also be used to treat high blood potassium levels. Salbutamol is usually used with an inhaler or nebulizer, but it is also available in a pill, liquid, and intravenous solution. Onset of action of the inhaled version is typically within 15 minutes and lasts for two to six hours.

Transplant rejection occurs when transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between donor and recipient and by use of immunosuppressant drugs after transplant.

In medicine, a nebulizer or nebuliser is a drug delivery device used to administer medication in the form of a mist inhaled into the lungs. Nebulizers are commonly used for the treatment of asthma, cystic fibrosis, COPD and other respiratory diseases or disorders. They use oxygen, compressed air or ultrasonic power to break up solutions and suspensions into small aerosol droplets that are inhaled from the mouthpiece of the device. An aerosol is a mixture of gas and solid or liquid particles.

Ipratropium bromide, sold under the trade name Atrovent among others, is a type of anticholinergic medication which opens up the medium and large airways in the lungs. It is used to treat the symptoms of chronic obstructive pulmonary disease and asthma. It is used by inhaler or nebulizer. Onset of action is typically within 15 to 30 minutes and lasts for three to five hours.

An inhaler is a medical device used for delivering medicines into the lungs through the work of a person's breathing. This allows medicines to be delivered to and absorbed in the lungs, which provides the ability for targeted medical treatment to this specific region of the body, as well as a reduction in the side effects of oral medications. There are a wide variety of inhalers, and they are commonly used to treat numerous medical conditions with asthma and chronic obstructive pulmonary disease (COPD) being among the most notable.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.

A metered-dose inhaler (MDI) is a device that delivers a specific amount of medication to the lungs, in the form of a short burst of aerosolized medicine that is usually self-administered by the patient via inhalation. It is the most commonly used delivery system for treating asthma, chronic obstructive pulmonary disease (COPD) and other respiratory diseases. The medication in a metered dose inhaler is most commonly a bronchodilator, corticosteroid or a combination of both for the treatment of asthma and COPD. Other medications less commonly used but also administered by MDI are mast cell stabilizers, such as cromoglicate or nedocromil.

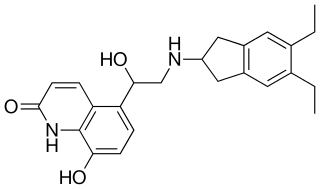
Levosalbutamol, also known as levalbuterol, is a short-acting β2 adrenergic receptor agonist used in the treatment of asthma and chronic obstructive pulmonary disease (COPD). Evidence is inconclusive regarding the efficacy of levosalbutamol versus salbutamol or salbutamol-levosalbutamol combinations, though levosalbutamol is believed to have a better safety profile due to its more selective binding to β2 receptors versus β1.
Tolypocladium inflatum is an ascomycete fungus originally isolated from a Norwegian soil sample that, under certain conditions, produces the immunosuppressant drug ciclosporin. In its sexual stage (teleomorph) it is a parasite on scarab beetles. It forms a small, compound ascocarp that arises from the cadaver of its host beetle. In its asexual stage (anamorph) it is a white mold that grows on soil. It is much more commonly found in its asexual stage and this is the stage that was originally given the name Tolypocladium inflatum.
The FKBPs, or FK506 binding proteins, constitute a family of proteins that have prolyl isomerase activity and are related to the cyclophilins in function, though not in amino acid sequence. FKBPs have been identified in many eukaryotes, ranging from yeast to humans, and function as protein folding chaperones for proteins containing proline residues. Along with cyclophilin, FKBPs belong to the immunophilin family.

A dry-powder inhaler (DPI) is a device that delivers medication to the lungs in the form of a dry powder. DPIs are commonly used to treat respiratory diseases such as asthma, bronchitis, emphysema and COPD although DPIs have also been used in the treatment of diabetes mellitus.

Pirbuterol is a short-acting β2 adrenoreceptor agonist with bronchodilating action used in the treatment of asthma, available as a breath-activated metered-dose inhaler.
Indacaterol is an ultra-long-acting beta-adrenoceptor agonist developed by Novartis. It needs to be taken only once a day, unlike the related drugs formoterol and salmeterol. It is licensed only for the treatment of chronic obstructive pulmonary disease (COPD). It is delivered as an aerosol formulation through a dry powder inhaler.
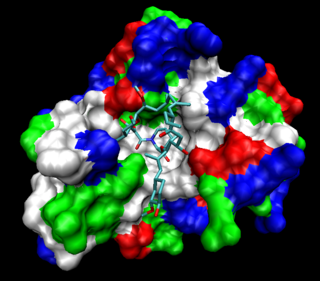
β2-adrenoceptor agonists are a group of drugs that act selectively on β2-receptors in the lungs causing bronchodilation. β2-agonists are used to treat asthma and COPD, diseases that cause obstruction in the airways. Prior to their discovery, the non-selective beta-agonist isoprenaline was used. The aim of the drug development through the years has been to minimise side effects, achieve selectivity and longer duration of action. The mechanism of action is well understood and has facilitated the development. The structure of the binding site and the nature of the binding is also well known, as is the structure activity relationship.

Pulmonary drug delivery is a route of administration in which patients use an inhaler to inhale their medications and drugs are absorbed into the bloodstream via the lung mucous membrane. This technique is most commonly used in the treatment of lung diseases, for example, asthma and chronic obstructive pulmonary disease (COPD). Different types of inhalers include metered-dose inhalers (MDI), dry powder inhalers (DPI), soft mist inhalers (SMI) and nebulizers. The rate and efficacy of pulmonary drug delivery are affected by drug particle properties, breathing patterns and respiratory tract geometry.
References
- ↑ Calne, R (Mar 2004). "Cyclosporine as a milestone in immunosuppression". Transplant. Proc. 36 (2 Suppl): 13S–15S. doi:10.1016/j.transproceed.2004.01.042. PMID 15041300.
- ↑ Madan V, Griffiths CE. "Systemic ciclosporin and tacrolimus in dermatology. Dermatol Ther. 2007 Jul-Aug;20(4):239-50.
- ↑ Kitahara K, Kawai S. "Cyclosporine and tacrolimus for the treatment of rheumatoid arthritis. Curr Opin Rheumatol. 2007 May;19(3):238-45. Review.
- ↑ Ridder, WH 3rd (Dec 2008). "Ciclosporin use in dry eye disease patients". Expert Opin Pharmacother. 9 (17): 3121–8. doi:10.1517/14656560802500613. PMID 19006483. S2CID 72181779.
- ↑ Czogalla, A (2009). "Oral cyclosporine A--the current picture of its liposomal and other delivery systems". Cell Mol Biol Lett. 14 (1): 139–52. doi:10.2478/s11658-008-0041-6. PMC 6275704 . PMID 19005620.
- 1 2 Iacono, AT; Smaldone, GC; Keenan, RJ; Diot, P; Dauber, JH; Zeevi, A; Burckart, GJ; Griffith, BP (May 1997). "Dose-related reversal of acute lung rejection by aerosolized cyclosporine". Am J Respir Crit Care Med. 155 (5): 1690–8. doi:10.1164/ajrccm.155.5.9154878. PMID 9154878.
- ↑ O'Riordan TG, Iacono A, Keenan RJ, Duncan SR, Burckart GJ, Griffith BP, Smaldone GC. "Delivery and distribution of aerosolized cyclosporine in lung allograft recipients. Am J Respir Crit Care Med. 1995 Feb;151 (2 Pt 1):516-21.
- ↑ Gilbert, BE; Wilson, SZ; Garcon, NM; Wyde, PR; Knight, V (Oct 1993). "Characterization and administration of cyclosporine liposomes as a small-particle aerosol". Transplantation. 56 (4): 974–7. doi: 10.1097/00007890-199310000-00037 . PMID 8212222. S2CID 39895268.
- ↑ Trammer, B; Amann, A; Haltner-Ukomadu, E; Tillmanns, S; Keller, M; Högger, P (Nov 2008). "Comparative permeability and diffusion kinetics of cyclosporine A liposomes and propylene glycol solution from human lung tissue into human blood ex vivo". Eur J Pharm Biopharm. 70 (3): 758–64. doi:10.1016/j.ejpb.2008.07.001. PMID 18656538.
- ↑ Tam, JM; McConville, JT; Williams, RO; Johnston, KP (Nov 2008). "Amorphous cyclosporin nanodispersions for enhanced pulmonary deposition and dissolution". J Pharm Sci. 97 (11): 4915–33. doi:10.1002/jps.21367. PMID 18351641.
- ↑ Fukaya, H; Iimura, A; Hoshiko, K; Fuyumuro, T; Noji, S; Nabeshima, T (Aug 2003). "A cyclosporin A/maltosyl-alpha-cyclodextrin complex for inhalation therapy of asthma". Eur Respir J. 22 (2): 213–9. doi: 10.1183/09031936.03.00018202 . PMID 12952250. S2CID 73731983.
- ↑ Zijlstra, GS; Rijkeboer, M; Jan; van Drooge, D; Sutter, M; Jiskoot, W; de Weert, M; Hinrichs, WL; Frijlink, HW (Jun 2007). "Characterization of a cyclosporine solid dispersion for inhalation". AAPS J. 9 (2): E190–9. doi:10.1208/aapsj0902021. PMC 2751408 . PMID 17614361.
- ↑ Myrdal, PB; Karlage, KL; Stein, SW; Brown, BA; Haynes, A (Apr 2004). "Optimized dose delivery of the peptide cyclosporine using hydrofluoroalkane-based metered dose inhalers". J Pharm Sci. 93 (4): 1054–61. doi:10.1002/jps.20025. PMID 14999741.
- ↑ Marijani, R; Shaik, MS; Chatterjee, A; Singh, M (Jan 2007). "Evaluation of metered dose inhaler (MDI) formulations of ciclosporin". J Pharm Pharmacol. 59 (1): 15–21. doi: 10.1211/jpp.59.1.0003 . PMID 17227616. S2CID 24608166.
- ↑ Evans, DJ; Cullinan, P; Geddes, DM (2001). "Cyclosporin as an oral corticosteroid sparing agent in stable asthma". Cochrane Database Syst Rev. 2010 (2): CD002993. doi:10.1002/14651858.CD002993. PMC 8407285 . PMID 11406057.
- ↑ Lock, SH; Kay, AB; Barnes, NC (Feb 1996). "Double-blind, placebo-controlled study of cyclosporin A as a corticosteroid-sparing agent in corticosteroid-dependent asthma". Am J Respir Crit Care Med. 153 (2): 509–14. doi:10.1164/ajrccm.153.2.8564089. PMID 8564089.
- ↑ Larché M, Robinson DS, Kay AB. "The role of T lymphocytes in the pathogenesis of asthma" J Allergy Clin Immunol 2003 Mar;111(3):450-63; quiz 464.
- ↑ Alexander, AG; Barnes, NC; Kay, AB; Corrigan, CJ (Apr 1995). "Clinical response to cyclosporin in chronic severe asthma is associated with reduction in serum soluble interleukin-2 receptor concentrations". Eur Respir J. 8 (4): 574–8. doi: 10.1183/09031936.95.08040574 . PMID 7664856. S2CID 18489547.
- ↑ Ezeamuzie, CI; Nwankwoala, RN (Jul 2000). "Allergen-induced bronchial eosinophilia in guinea-pigs is inhibited by both pre- and post-induction cyclosporin-A treatments". Int J Immunopharmacol. 22 (7): 515–22. doi:10.1016/s0192-0561(00)00015-1. PMID 10785548.
- ↑ Khan LN, Kon OM, Macfarlane AJ, Meng Q, Ying S, Barnes NC, Kay AB. "Attenuation of the allergen-induced late asthmatic reaction by cyclosporin A is associated with inhibition of bronchial eosinophils, interleukin-5, granulocyte macrophage colony-stimulating factor, and eotaxin.
- ↑ Kay, AB (May 1994). "Immunosuppressive agents in chronic severe asthma". Allergy Proc. 15 (3): 147–50. doi:10.2500/108854194778702838. PMID 7523242.
- ↑ Katz, A; Coran, AG; Oldham, KT; Guice, KS (Jun 1993). "Decreased oxidized glutathione with aerosolized cyclosporine delivery" (PDF). J Surg Res. 54 (6): 597–602. doi:10.1006/jsre.1993.1091. hdl:2027.42/30777. PMID 8412070.
- ↑ Xie, QM; Chen, JQ; Shen, WH; Yang, QH; Bian, RL (Mar 2002). "Effects of cyclosporin A by aerosol on airway hyperresponsiveness and inflammation in guinea pigs". Acta Pharmacol. Sin. 23 (3): 243–7. PMID 11918849.
- ↑ Arima, M; Yukawa, T; Terashi, Y; Makino, S (Dec 1994). "Effect of inhaled cyclosporin A on the allergen-induced late asthmatic response and increased in airway hyperresponsiveness in a guinea pig model of asthma". Arerugi. 43 (11): 1316–25. PMID 7887807.
- ↑ Rohatagi, S; Calic, F; Harding, N; Ozoux, ML; Bouriot, JP; Kirkesseli, S; DeLeij, L; Jensen, BK (Nov 2000). "Pharmacokinetics, pharmacodynamics, and safety of inhaled cyclosporin A (ADI628) after single and repeated administration in healthy male and female subjects and asthmatic patients". J Clin Pharmacol. 40 (11): 1211–26. doi:10.1177/009127000004001106. PMID 11075307. S2CID 10004392.
- ↑ Gaga, M; Zervas, E; Grivas, S; Castro, M; Chanez, P (2007). "Evaluation and management of severe asthma". Curr. Med. Chem. 14 (9): 1049–59. doi:10.2174/092986707780362961. PMID 17439402.
- ↑ Barnes, PJ (Aug 1996). "Immunomodulation as asthma therapy: where do we stand?". Eur Respir J Suppl. 22: 154S–159S. PMID 8871062.
- ↑ Arcasoy, SM (Dec 2004). "Medical complications and management of lung transplant recipients". Respir Care Clin N Am. 10 (4): 505–29. doi:10.1016/j.rcc.2004.06.002. PMID 15585180.
- ↑ Bando, K; Paradis, IL; Komatsu, K; Konishi, H; Matsushima, M; Keena, RJ; Hardesty, RL; Armitage, JM; Griffith, BP (Jan 1995). "Analysis of time-dependent risks for infection, rejection, and death after pulmonary transplantation". J Thorac Cardiovasc Surg. 109 (1): 49–57. doi: 10.1016/s0022-5223(95)70419-1 . PMID 7815807.
- ↑ Dowling, RD; Zenati, M; Burckart, GJ; Yousem, SA; Schaper, M; Simmons, RL; Hardesty, RL; Griffith, BP (Aug 1990). "Aerosolized cyclosporine as single-agent immunotherapy in canine lung allografts". Surgery. 108 (2): 198–204. PMID 2382220.
- ↑ Keenan, RJ; Duncan, AJ; Yousem, SA; Zenati, M; Schaper, M; Dowling, RD; Alarie, Y; Burckart, GJ; Griffith, BP (Jan 1992). "Improved immunosuppression with aerosolized cyclosporine in experimental pulmonary transplantation". Transplantation. 53 (1): 20–5. doi: 10.1097/00007890-199201000-00003 . PMID 1733067. S2CID 12010964.
- ↑ Blot F, Tavakoli R, Sellam S, Epardeau B, Faurisson F, Bernard N, Becquemin MH, Frachon I, Stern M, Pocidalo JJ, et al. "Nebulized cyclosporine for prevention of acute pulmonary allograft rejection in the rat: pharmacokinetic and histologic study. J Heart Lung Transplant. 1995 Nov-Dec;14 (6 Pt 1):1162-72.
- ↑ Keenan, RJ; Iacono, A; Dauber, JH; Zeevi, A; Yousem, SA; Ohori, NP; Burckart, GJ; Kawai, A; Smaldone, GC; Griffith, BP (Feb 1997). "Treatment of refractory acute allograft rejection with aerosolized cyclosporine in lung transplant recipients". J Thorac Cardiovasc Surg. 113 (2): 335–40. doi: 10.1016/s0022-5223(97)70331-3 . PMID 9040628.
- ↑ McCurry, KR; Iacono, AT; Dauber, JH; Grgurich, WF; Pham, SM; Hattler, BG; Keenan, RJ; Griffith, BP. "Lung and heart-lung transplantation at the University of Pittsburgh". Clin Transpl. 1997: 209–18.
- ↑ Iacono, AT; Johnson, BA; Grgurich, WF; Youssef, JG; Corcoran, TE; Seiler, DA; Dauber, JH; Smaldone, GC; Zeevi, A; Yousem, SA; Fung, JJ; Burckart, GJ; McCurry, KR; Griffith, BP (Jan 2006). "A randomized trial of inhaled cyclosporine in lung-transplant recipients". N Engl J Med. 354 (2): 141–50. doi: 10.1056/nejmoa043204 . PMID 16407509. S2CID 33787892.
- ↑ Martinu, T; Chen, DF; Palmer, SM (Jan 2009). "Acute rejection and humoral sensitization in lung transplant recipients". Proceedings of the American Thoracic Society. 6 (1): 54–65. doi:10.1513/pats.200808-080go. PMC 2626504 . PMID 19131531.
- ↑ Belperio, JA; Weigt, SS; Fishbein, MC; Lynch, JP (Jan 2009). "Chronic lung allograft rejection: mechanisms and therapy". Proceedings of the American Thoracic Society. 6 (1): 108–21. doi:10.1513/pats.200807-073go. PMID 19131536. S2CID 23071315.
- ↑ Orens, JB; Garrity, ER Jr (Jan 2009). "General overview of lung transplantation and review of organ allocation". Proceedings of the American Thoracic Society. 6 (1): 13–9. doi:10.1513/pats.200807-072go. PMID 19131526.
- ↑ "Ciclosporin clinical trials". Clinicaltrials.gov. Retrieved 3 June 2011.
- ↑ Knight, V; Koshkina, NV; Golunski, E; Roberts, LE; Gilbert, BE (2004). "Cyclosporin an aerosol improves the anticancer effect of Paclitaxel aerosol in mice". Trans Am Clin Climatol Assoc. 115: 395–404. PMC 2263789 . PMID 17060982.