The sievert is a unit in the International System of Units (SI) intended to represent the stochastic health risk of ionizing radiation, which is defined as the probability of causing radiation-induced cancer and genetic damage. The sievert is important in dosimetry and radiation protection. It is named after Rolf Maximilian Sievert, a Swedish medical physicist renowned for work on radiation dose measurement and research into the biological effects of radiation.
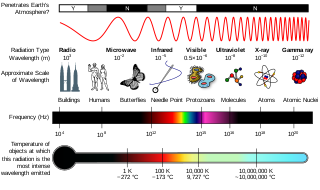
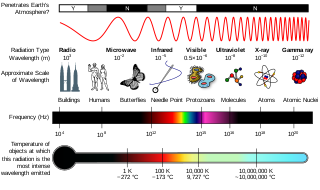
Ionizing radiation, including nuclear radiation, consists of subatomic particles or electromagnetic waves that have sufficient energy to ionize atoms or molecules by detaching electrons from them. Some particles can travel up to 99% of the speed of light, and the electromagnetic waves are on the high-energy portion of the electromagnetic spectrum.
Radiation dosimetry in the fields of health physics and radiation protection is the measurement, calculation and assessment of the ionizing radiation dose absorbed by an object, usually the human body. This applies both internally, due to ingested or inhaled radioactive substances, or externally due to irradiation by sources of radiation.
Radiation protection, also known as radiological protection, is defined by the International Atomic Energy Agency (IAEA) as "The protection of people from harmful effects of exposure to ionizing radiation, and the means for achieving this". Exposure can be from a source of radiation external to the human body or due to internal irradiation caused by the ingestion of radioactive contamination.
Equivalent dose is a dose quantity H representing the stochastic health effects of low levels of ionizing radiation on the human body which represents the probability of radiation-induced cancer and genetic damage. It is derived from the physical quantity absorbed dose, but also takes into account the biological effectiveness of the radiation, which is dependent on the radiation type and energy. In the SI system of units, the unit of measure is the sievert (Sv).

Health physics, also referred to as the science of radiation protection, is the profession devoted to protecting people and their environment from potential radiation hazards, while making it possible to enjoy the beneficial uses of radiation. Health physicists normally require a four-year bachelor’s degree and qualifying experience that demonstrates a professional knowledge of the theory and application of radiation protection principles and closely related sciences. Health physicists principally work at facilities where radionuclides or other sources of ionizing radiation are used or produced; these include research, industry, education, medical facilities, nuclear power, military, environmental protection, enforcement of government regulations, and decontamination and decommissioning—the combination of education and experience for health physicists depends on the specific field in which the health physicist is engaged.
Absorbed dose is a dose quantity which is the measure of the energy deposited in matter by ionizing radiation per unit mass. Absorbed dose is used in the calculation of dose uptake in living tissue in both radiation protection, and radiology. It is also used to directly compare the effect of radiation on inanimate matter such as in radiation hardening.

Radioactive contamination, also called radiological pollution, is the deposition of, or presence of radioactive substances on surfaces or within solids, liquids, or gases, where their presence is unintended or undesirable.
ALARP, or ALARA, is a principle in the regulation and management of safety-critical and safety-involved systems. The principle is that the residual risk shall be reduced as far as reasonably practicable. In UK and NZ Health and Safety law, it is equivalent to SFAIRP. In the US, ALARA is used in the regulation of radiation risks.
The International Commission on Radiological Protection (ICRP) is an independent, international, non-governmental organization, with the mission to protect people, animals, and the environment from the harmful effects of ionising radiation. Its recommendations form the basis of radiological protection policy, regulations, guidelines and practice worldwide.

The Control of Substances Hazardous to Health Regulations 2002 is a United Kingdom Statutory Instrument which states general requirements imposed on employers to protect employees and other persons from the hazards of substances used at work by risk assessment, control of exposure, health surveillance and incident planning. There are also duties on employees to take care of their own exposure to hazardous substances and prohibitions on the import of certain substances into the European Economic Area. The regulations reenacted, with amendments, the Control of Substances Hazardous to Work Regulations 1999 and implement several European Union directives.
The European Committee on Radiation Risk (ECRR) is an informal committee formed in 1997 following a meeting by the European Green Party at the European Parliament to review the Council of Europe's directive 96/29Euratom, issued in May of the previous year. ECRR is not a formal scientific advisory committee to the European Commission or to the European Parliament. Its report is published by the Green Audit. Dr. Busby is the secretary of ECRR.
Radiobiology is a field of clinical and basic medical sciences that involves the study of the effects of ionizing radiation on living things, in particular health effects of radiation. Ionizing radiation is generally harmful and potentially lethal to living things but can have health benefits in radiation therapy for the treatment of cancer and thyrotoxicosis. Its most common impact is the induction of cancer with a latent period of years or decades after exposure. High doses can cause visually dramatic radiation burns, and/or rapid fatality through acute radiation syndrome. Controlled doses are used for medical imaging and radiotherapy.
Internal dosimetry is the science and art of internal ionising radiation dose assessment due to radionuclides incorporated inside the human body.

The roentgen or röntgen is a legacy unit of measurement for the exposure of X-rays and gamma rays, and is defined as the electric charge freed by such radiation in a specified volume of air divided by the mass of that air . In 1928, it was adopted as the first international measurement quantity for ionizing radiation to be defined for radiation protection, as it was then the most easily replicated method of measuring air ionization by using ion chambers. It is named after the German physicist Wilhelm Röntgen, who discovered X-rays and was awarded the first Nobel Prize in Physics for the discovery.
Effective dose is a dose quantity in the International Commission on Radiological Protection (ICRP) system of radiological protection.
Optical radiation is part of the electromagnetic spectrum. It is a type of non-ionising radiation (NIR), with electromagnetic fields (EMFs).
The committed dose in radiological protection is a measure of the stochastic health risk due to an intake of radioactive material into the human body. Stochastic in this context is defined as the probability of cancer induction and genetic damage, due to low levels of radiation. The SI unit of measure is the sievert.
Radiation exposure is a measure of the ionization of air due to ionizing radiation from photons. It is defined as the electric charge freed by such radiation in a specified volume of air divided by the mass of that air. As of 2007, "medical radiation exposure" was defined by the International Commission on Radiological Protection as exposure incurred by people as part of their own medical or dental diagnosis or treatment; by persons, other than those occupationally exposed, knowingly, while voluntarily helping in the support and comfort of patients; and by volunteers in a programme of biomedical research involving their exposure. Common medical tests and treatments involving radiation include X-rays, CT scans, mammography, lung ventilation and perfusion scans, bone scans, cardiac perfusion scan, angiography, radiation therapy, and more. Each type of test carries its own amount of radiation exposure. There are two general categories of adverse health effects caused by radiation exposure: deterministic effects and stochastic effects. Deterministic effects are due to the killing/malfunction of cells following high doses; and stochastic effects involve either cancer development in exposed individuals caused by mutation of somatic cells, or heritable disease in their offspring from mutation of reproductive (germ) cells.
The European Federation of Organisations for Medical Physics (EFOMP) was founded in May 1980 in London to serve as an umbrella organisation representing the national Medical Physics societies in Europe. The office moved to Utrecht in January 2021. It is a non-profit organisation and aims to foster and coordinate the activities of its national member organisations, encourage exchange and dissemination of professional and scientific information, develop guidelines for education, training and accreditation programmes and to make recommendations on the responsibilities, organisational relationships and roles of medical physicists.