Hepatitis is inflammation of the liver tissue. Some people or animals with hepatitis have no symptoms, whereas others develop yellow discoloration of the skin and whites of the eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pain, and diarrhea. Hepatitis is acute if it resolves within six months, and chronic if it lasts longer than six months. Acute hepatitis can resolve on its own, progress to chronic hepatitis, or (rarely) result in acute liver failure. Chronic hepatitis may progress to scarring of the liver (cirrhosis), liver failure, and liver cancer.
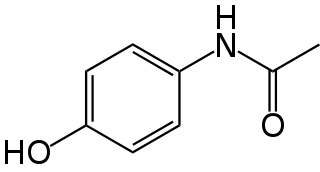
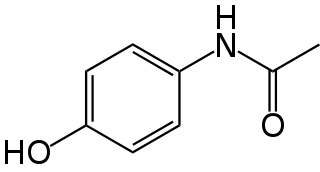
Paracetamol is a non-opioid analgesic and antipyretic agent used to treat fever and mild to moderate pain. It is a widely used over the counter medication. Common brand names include Tylenol and Panadol.
Liver function tests, also referred to as a hepatic panel, are groups of blood tests that provide information about the state of a patient's liver. These tests include prothrombin time (PT/INR), activated partial thromboplastin time (aPTT), albumin, bilirubin, and others. The liver transaminases aspartate transaminase and alanine transaminase are useful biomarkers of liver injury in a patient with some degree of intact liver function.

Alcoholic liver disease (ALD), also called alcohol-related liver disease (ARLD), is a term that encompasses the liver manifestations of alcohol overconsumption, including fatty liver, alcoholic hepatitis, and chronic hepatitis with liver fibrosis or cirrhosis.

Hepatotoxicity implies chemical-driven liver damage. Drug-induced liver injury is a cause of acute and chronic liver disease caused specifically by medications and the most common reason for a drug to be withdrawn from the market after approval.

Budd–Chiari syndrome is a very rare condition, affecting one in a million adults. The condition is caused by occlusion of the hepatic veins that drain the liver. The symptoms are non-specific and vary widely, but it may present with the classical triad of abdominal pain, ascites, and liver enlargement. It is usually seen in younger adults, with the median age at diagnosis between the ages of 35 and 40, and it has a similar incidence in males and females. The syndrome can be fulminant, acute, chronic, or asymptomatic. Subacute presentation is the most common form.

Alcoholic hepatitis is hepatitis due to excessive intake of alcohol. Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8–10 drinks per day. It is usually found in association with fatty liver, an early stage of alcoholic liver disease, and may contribute to the progression of fibrosis, leading to cirrhosis. Symptoms may present acutely after a large amount of alcoholic intake in a short time period, or after years of excess alcohol intake. Signs and symptoms of alcoholic hepatitis include jaundice, ascites, fatigue and hepatic encephalopathy. Mild cases are self-limiting, but severe cases have a high risk of death. Severe cases may be treated with glucocorticoids. The condition often comes on suddenly and may progress in severity very rapidly.

Autoimmune hepatitis, formerly known as lupoid hepatitis, plasma cell hepatitis, or autoimmune chronic active hepatitis, is a chronic, autoimmune disease of the liver that occurs when the body's immune system attacks liver cells, causing the liver to be inflamed. Common initial symptoms may include fatigue, nausea, muscle aches, or weight loss or signs of acute liver inflammation including fever, jaundice, and right upper quadrant abdominal pain. Individuals with autoimmune hepatitis often have no initial symptoms and the disease may be detected by abnormal liver function tests and increased protein levels during routine bloodwork or the observation of an abnormal-looking liver during abdominal surgery.

Amanita virosa is a species of fungus in the class Agaricomycetes. In the UK, it has the recommended English name of destroying angel and is known internationally as the European destroying angel. Basidiocarps are agaricoid (mushroom-shaped) and pure white with an ring on the stem and a sack-like volva at the base. The species is deadly poisonous. It occurs in Europe and northern Asia. Amanita virosa was formerly reported from North America, but research has shown that similar-looking American species, including Amanita bisporigera and A. ocreata, are distinct.

Acute liver failure is the appearance of severe complications rapidly after the first signs of liver disease, and indicates that the liver has sustained severe damage. The complications are hepatic encephalopathy and impaired protein synthesis. The 1993 classification defines hyperacute as within 1 week, acute as 8–28 days, and subacute as 4–12 weeks; both the speed with which the disease develops and the underlying cause strongly affect outcomes.

Hepatorenal syndrome is a life-threatening medical condition that consists of rapid deterioration in kidney function in individuals with cirrhosis or fulminant liver failure. HRS is usually fatal unless a liver transplant is performed, although various treatments, such as dialysis, can prevent advancement of the condition.
Chronic liver disease in the clinical context is a disease process of the liver that involves a process of progressive destruction and regeneration of the liver parenchyma leading to fibrosis and cirrhosis. "Chronic liver disease" refers to disease of the liver which lasts over a period of six months. It consists of a wide range of liver pathologies which include inflammation, liver cirrhosis, and hepatocellular carcinoma. The entire spectrum need not be experienced.

NAPQI, also known as NAPBQI or N-acetyl-p-benzoquinone imine, is a toxic byproduct produced during the xenobiotic metabolism of the analgesic paracetamol (acetaminophen). It is normally produced only in small amounts, and then almost immediately detoxified in the liver.
Acute fatty liver of pregnancy is a rare life-threatening complication of pregnancy that occurs in the third trimester or the immediate period after delivery. It is thought to be caused by a disordered metabolism of fatty acids by mitochondria in the fetus, caused by long-chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency. This leads to decreased metabolism of long chain fatty acids by the feto-placental unit, causing subsequent rise in hepatotoxic fatty acids in maternal plasma. The condition was previously thought to be universally fatal, but aggressive treatment by stabilizing the mother with intravenous fluids and blood products in anticipation of early delivery has improved prognosis.

Liver failure is the inability of the liver to perform its normal synthetic and metabolic functions as part of normal physiology. Two forms are recognised, acute and chronic (cirrhosis). Recently, a third form of liver failure known as acute-on-chronic liver failure (ACLF) is increasingly being recognized.
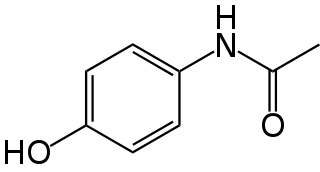
Paracetamol poisoning, also known as acetaminophen poisoning, is caused by excessive use of the medication paracetamol (acetaminophen). Most people have few or non-specific symptoms in the first 24 hours following overdose. These symptoms include feeling tired, abdominal pain, or nausea. This is typically followed by absence of symptoms for a couple of days, after which yellowish skin, blood clotting problems, and confusion occurs as a result of liver failure. Additional complications may include kidney failure, pancreatitis, low blood sugar, and lactic acidosis. If death does not occur, people tend to recover fully over a couple of weeks. Without treatment, death from toxicity occurs 4 to 18 days later.

Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage to the liver leads to repair of liver tissue and subsequent formation of scar tissue. Over time, scar tissue can replace normal functioning tissue, leading to the impaired liver function of cirrhosis. The disease typically develops slowly over months or years. Early symptoms may include tiredness, weakness, loss of appetite, unexplained weight loss, nausea and vomiting, and discomfort in the right upper quadrant of the abdomen. As the disease worsens, symptoms may include itchiness, swelling in the lower legs, fluid build-up in the abdomen, jaundice, bruising easily, and the development of spider-like blood vessels in the skin. The fluid build-up in the abdomen may develop into spontaneous infections. More serious complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus, stomach, or intestines, and liver cancer.Stages of cirrhosis include compensated cirrhosis and decompensated cirrhosis.

The Rumack–Matthew nomogram, also known as the acetaminophen nomogram, is an acetaminophen toxicity nomogram. It plots serum concentration of acetaminophen against the time since ingestion, in order to predict possible liver toxicity and allow a clinician to decide whether to proceed with N-Acetylcysteine (NAC) treatment. It is a logarithmic graph starting 4 hours after ingestion; at this time the absorption of acetaminophen is considered likely to be complete.
A liver support system or diachysis is a type of therapeutic device to assist in performing the functions of the liver. Such systems focus either on removing the accumulating toxins, or providing additional replacement of the metabolic functions of the liver through the inclusion of hepatocytes to the device. This system is in trial to help people with acute liver failure (ALF) or acute-on-chronic liver failure.

Liver angiosarcoma also known as angiosarcoma of the liver or hepatic angiosarcoma is a rare and rapidly fatal cancer arising from endothelial that line the blood vessels of the liver. It is a type of angiosarcoma. Although very rare with around 200 cases diagnosed each year, it is still considered the third most common primary liver cancer, making up around 2% of all primary liver cancers. Liver angiosarcoma can be primary, meaning it arose in the liver, or secondary, meaning the angiosarcoma arose elsewhere and metastasized to the liver. This article covers PHA, however much is also applicable to secondary tumors.