Related Research Articles

Leprosy, also known as Hansen's disease (HD), is a long-term infection by the bacteria Mycobacterium leprae or Mycobacterium lepromatosis. Infection can lead to damage of the nerves, respiratory tract, skin, and eyes. This nerve damage may result in a lack of ability to feel pain, which can lead to the loss of parts of a person's extremities from repeated injuries or infection through unnoticed wounds. An infected person may also experience muscle weakness and poor eyesight. Leprosy symptoms may begin within one year, but, for some people, symptoms may take 20 years or more to occur.

The Mantoux test or Mendel–Mantoux test is a tool for screening for tuberculosis (TB) and for tuberculosis diagnosis. It is one of the major tuberculin skin tests used around the world, largely replacing multiple-puncture tests such as the tine test. The Heaf test, a form of tine test, was used until 2005 in the UK, when it was replaced by the Mantoux test. The Mantoux test is endorsed by the American Thoracic Society and Centers for Disease Control and Prevention. It was also used in the USSR and is now prevalent in most of the post-Soviet states, although Soviet mantoux produced many false positives due to children's allergic reaction.
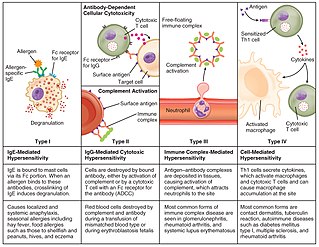
Hypersensitivity is an abnormal physiological condition in which there is an undesirable and adverse immune response to antigen. It is an abnormality in the immune system that causes immune diseases including allergies and autoimmunity. It is caused by many types of particles and substances from the external environment or from within the body that are recognized by the immune cells as antigens. The immune reactions are usually referred to as an over-reaction of the immune system and they are often damaging and uncomfortable.
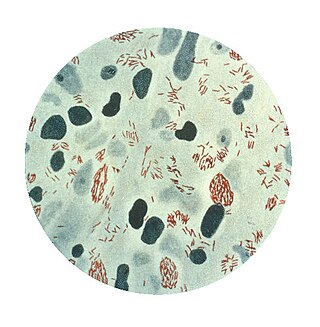
Mycobacterium leprae is one of the two species of bacteria that cause Hansen’s disease (leprosy), a chronic but curable infectious disease that damages the peripheral nerves and targets the skin, eyes, nose, and muscles.
The Heaf test, a diagnostic skin test, was long performed to determine whether or not children had been exposed to tuberculosis infection. The test was named after F. R. G. Heaf. Also known as the Sterneedle test, it was administered by a Heaf gun, a spring-loaded instrument with six needles arranged in a circular formation which was inserted in the wrist or shoulder.
The direct and indirect Coombs tests, also known as antiglobulin test (AGT), are blood tests used in immunohematology. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells. Since these antibodies sometimes destroy red blood cells they can cause anemia; this test can help clarify the condition. The indirect Coombs test detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells; the test can be carried out to diagnose reactions to a blood transfusion.

Neuritis is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
Latent tuberculosis (LTB), also called latent tuberculosis infection (LTBI) is when a person is infected with Mycobacterium tuberculosis, but does not have active tuberculosis (TB). Active tuberculosis can be contagious while latent tuberculosis is not, and it is therefore not possible to get TB from someone with latent tuberculosis. The main risk is that approximately 10% of these people will go on to develop active tuberculosis. This is particularly true, and there is added risk, in particular situations such as medication that suppresses the immune system or advancing age.
The Fernandez reaction is a reaction that occurs to signal a positive result in the lepromin skin test for leprosy. The reaction occurs in the skin at the site of injection if the body possesses antibodies to the Dharmendra antigen, one of the antigens found in Mycobacterium leprae, the bacteria that causes leprosy. The reaction occurs via a delayed-type hypersensitivity mechanism. This reaction occurs within 48 hours of injection of lepromin and is seen in only tuberculoid forms of leprosy. This represents a delayed-type hypersensitivity reaction. In contrast, the Mitsuda reaction occurs 3–4 weeks after injection of lepromin and is only seen in patients with the tuberculoid form of leprosy. In terms of mechanism of action and appearance, the reaction is similar to the tuberculin reaction of a positive Mantoux test for tuberculosis.

Type III hypersensitivity, in the Gell and Coombs classification of allergic reactions, occurs when there is accumulation of immune complexes that have not been adequately cleared by innate immune cells, giving rise to an inflammatory response and attraction of leukocytes. There are three steps that lead to this response. The first step is immune complex formation, which involves the binding of antigens to antibodies to form mobile immune complexes. The second step is immune complex deposition, during which the complexes leave the plasma and are deposited into tissues. Finally, the third step is the inflammatory reaction, during which the classical pathway is activated and macrophages and neutrophils are recruited to the affected tissues. Such reactions may progress to immune complex diseases.
A leprostatic agent is a drug that interferes with proliferation of the bacterium that causes leprosy.
This page is currently under construction.

Lepromatous leprosy is a form of leprosy characterized by pale macules in the skin.
Mycobacterium lepromatosis is an aerobic, acid-fast bacillus (AFB), and the second known causative agent of Hansen's disease (leprosy). It was discovered in 2008. Analysis of the 16S rRNA gene confirms that the species is distinct from Mycobacterium leprae.
William Jopling was an Italian-born British leprologist who together with D. S. Ridley proposed the Ridley-Jopling classification of leprosy (1962), and wrote the widely read textbook of "Handbook of Leprosy" which had a fifth edition. He had a wide understanding of leprosy problems based on his experiences as the director of Jordan hospital, a leprosy hospital (1950–1967) in England and wrote various articles including "leprosy stigma".

Kensuke Mitsuda was a Japanese leprologist and director of the Tama Zenshoen Sanatorium (1914–1931) and the National Sanatorium Nagashima Aiseien (1931–1957). He had been at the frontier of leprosy policy of Japan. He was given the Order of Cultural Merits (1951) and Damien-Dutton Award (1961). He has been the cause of admiration from one side, and the target of criticism from the other.
Mosuke Murata was a Japanese dermatologist and was the designator of erythema nodosum leprosum (ENL)(1912), the type 2 lepra reaction.
Fumio Hayashi was a Japanese physician and leprologist. He worked in Tama Zenshoen Sanatorium, Nagashima Aiseien Sanatorium, Hoshizuka Keiaien Sanatorium and Ooshima Seishoen Sanatorium. He helped with Kensuke Mitsuda, and completed the first lepromin test or Mitsuda skin test.
Lucio's phenomenon is an unusual reaction seen almost exclusively in patients from the Caribbean and Mexico with diffuse lepromatous leprosy, especially in untreated cases. It is characterised by recurrent crops of large, sharply demarcated, ulcerative lesions, affecting mainly the lower extremities, but may generalise and become fatal as a result of secondary bacterial infection and sepsis.
Paul Bargehr was an Austrian medical doctor and writer mostly known for his work treating Hansen's disease (leprosy) in the Dutch East Indies. Although the Japanese researcher Kensuke Mitsuda receives credit for first developing the modern lepromin test for distinguishing between different forms of Hansen's disease, Bargehr's work was responsible for coining and popularizing its current name.
References
- ↑ "Leprosy". The Lecturio Medical Concept Library. Retrieved 1 August 2021.
- ↑ Dermatologic Manifestations of Leprosy~workup at eMedicine
- ↑ "Ridley Jopling" . Retrieved 11 December 2014.
- ↑ "Mitsuda Reaction" . Retrieved 11 December 2014.
- ↑ "Lepromin test & Dharmendra antigen". 2008-10-23. Retrieved 11 December 2014.
- ↑ Feldman & al. (1951), p. 53.
- ↑ Castellani, Aldo (1948), "The Relative Importance in Practice of Various Laboratory Methods in the Diagnosis of Leprosy", Memoria del V Congreso Internacional de la Lepra.
- ↑ Mitsuda, K (1919). "On the Value of Skin Reaction with Emulsion of Leproma". Japanese Journal of Dermatology. 19: 697–708.
- ↑ Outlook of the 3rd International Leprosy Conference(1950) Sato S. Papers of Kensuke Mitsuda, 2nd edition, Okayama, Japan
- ↑ Feldman, William H.; Karlson, Alfred G.; Grindlay, John H. (March 1951), "Lepromin: Mitsuda's Reaction with Experimental Observations in Dogs", Annals of the New York Academy of Sciences, New York City: NYAS, 54 (1): 53–72, Bibcode:1951NYASA..54...53F, doi:10.1111/j.1749-6632.1951.tb45832.x, PMID 14819908 .
- ↑ Hayashi, F (1933). "Mitsuda's Skin Reaction in Leprosy". Int J Leprosy. 1: 31–8.