Related Research Articles

Spina bifida /ˌspaɪnə ˈbɪfɪdə/ is a birth defect in which there is incomplete closing of the spine and the membranes around the spinal cord during early development in pregnancy. There are three main types: spina bifida occulta, meningocele and myelomeningocele. Meningocele and myelomeningocele may be grouped as spina bifida cystica. The most common location is the lower back, but in rare cases it may be in the middle back or neck.

Iniencephaly is a rare type of cephalic disorder characterised by three common characteristics: a defect to the occipital bone, spina bifida of the cervical vertebrae and retroflexion of the head on the cervical spine. Stillbirth is the most common outcome, with a few rare examples of live birth, after which death invariably occurs within a short time.

Prenatal testing is a tool that can be used to detect some birth defects at various stages prior to birth. Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible. These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts or as early in gestation as practicable. Screening can detect problems such as neural tube defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Down syndrome, trisomy 18, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems which primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.

Omphalocele or omphalocoele also called exomphalos, is a rare abdominal wall defect. Beginning at the 6th week of development, rapid elongation of the gut and increased liver size reduces intra abdominal space, which pushes intestinal loops out of the abdominal cavity. Around 10th week, the intestine returns to the abdominal cavity and the process is completed by the 12th week. Persistence of intestine or the presence of other abdominal viscera in the umbilical cord results in an omphalocele.
A hysterotomy is an incision made in the uterus. This surgical incision is used in several medical procedures, including during termination of pregnancy in the second trimester and delivering the fetus during caesarean section. It is also used to gain access and perform surgery on a fetus during pregnancy to correct birth defects, and it is an option to achieve resuscitation if cardiac arrest occurs during pregnancy and it is necessary to remove the fetus from the uterus.
Fetoscopy is an endoscopic procedure during pregnancy to allow surgical access to the fetus, the amniotic cavity, the umbilical cord, and the fetal side of the placenta. A small (3–4 mm) incision is made in the abdomen, and an endoscope is inserted through the abdominal wall and uterus into the amniotic cavity. Fetoscopy allows for medical interventions such as a biopsy or a laser occlusion of abnormal blood vessels or the treatment of spina bifida.
Prenatal development includes the development of the embryo and of the fetus during a viviparous animal's gestation. Prenatal development starts with fertilization, in the germinal stage of embryonic development, and continues in fetal development until birth.

Hand of Hope is a 1999 medical photograph taken by Michael Clancy during open fetal surgery, showing the hand of the fetus extending from the incision in the mother's uterus and seeming to grasp a surgeon's finger. Clancy was documenting a procedure being developed at Vanderbilt University to treat spina bifida. The photograph was taken on 19 August and the baby was safely delivered on 2 December.

Neural tube defects (NTDs) are a group of birth defects in which an opening in the spine or cranium remains from early in human development. In the third week of pregnancy called gastrulation, specialized cells on the dorsal side of the embryo begin to change shape and form the neural tube. When the neural tube does not close completely, an NTD develops.

Fetal surgery also known as antenatal surgery, prenatal surgery, is a growing branch of maternal-fetal medicine that covers any of a broad range of surgical techniques that are used to treat congenital abnormalities in fetuses who are still in the pregnant uterus. There are three main types: open fetal surgery, which involves completely opening the uterus to operate on the fetus; minimally invasive fetoscopic surgery, which uses small incisions and is guided by fetoscopy and sonography; and percutaneous fetal therapy, which involves placing a catheter under continuous ultrasound guidance.

The EXIT procedure, or ex utero intrapartum treatment procedure, is a specialized surgical delivery procedure used to deliver babies who have airway compression. Causes of airway compression in newborn babies result from a number of rare congenital disorders, including bronchopulmonary sequestration, congenital cystic adenomatoid malformation, mouth or neck tumor such as teratoma, and lung or pleural tumor such as pleuropulmonary blastoma. Airway compression discovered at birth is a medical emergency. In many cases, however, the airway compression is discovered during prenatal ultrasound exams, permitting time to plan a safe delivery using the EXIT procedure or other means.

Ventriculomegaly is a brain condition that mainly occurs in the fetus when the lateral ventricles become dilated. The most common definition uses a width of the atrium of the lateral ventricle of greater than 10 mm. This occurs in around 1% of pregnancies. When this measurement is between 10 and 15 mm, the ventriculomegaly may be described as mild to moderate. When the measurement is greater than 15mm, the ventriculomegaly may be classified as more severe.
The Fetal Treatment Center at the University of California, San Francisco is a multidisciplinary care center dedicated to the diagnosis, treatment, and long-term follow-up of fetal birth defects. It combines the talents of specialists in pediatric surgery, genetics, obstetrics/perinatology, radiology, nursing, and neonatal medicine.

Rachischisis is a developmental birth defect involving the neural tube. This anomaly occurs in utero, when the posterior neuropore of the neural tube fails to close by the 27th intrauterine day. As a consequence the vertebrae overlying the open portion of the spinal cord do not fully form and remain unfused and open, leaving the spinal cord exposed. Patients with rachischisis have motor and sensory deficits, chronic infections, and disturbances in bladder function. This defect often occurs with anencephaly.
A fetus or foetus is the unborn offspring that develops from a mammal embryo. Following embryonic development, the fetal stage of development takes place. In human prenatal development, fetal development begins from the ninth week after fertilization and continues until the birth of a newborn. Prenatal development is a continuum, with no clear defining feature distinguishing an embryo from a fetus. However, a fetus is characterized by the presence of all the major body organs, though they will not yet be fully developed and functional and some not yet situated in their final anatomical location.

Spinal disease refers to a condition impairing the backbone. These include various diseases of the back or spine ("dorso-"), such as kyphosis. Dorsalgia refers to back pain. Some other spinal diseases include spinal muscular atrophy, ankylosing spondylitis, lumbar spinal stenosis, spina bifida, spinal tumors, osteoporosis and cauda equina syndrome.
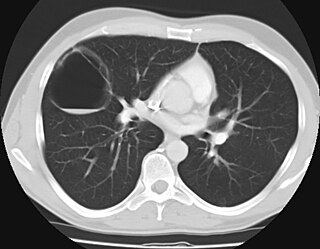
Congenital pulmonary airway malformation (CPAM), formerly known as congenital cystic adenomatoid malformation (CCAM), is a congenital disorder of the lung similar to bronchopulmonary sequestration. In CPAM, usually an entire lobe of lung is replaced by a non-working cystic piece of abnormal lung tissue. This abnormal tissue will never function as normal lung tissue. The underlying cause for CPAM is unknown. It occurs in approximately 1 in every 30,000 pregnancies.

Memorial Hermann–Texas Medical Center is a nationally ranked hospital at the Texas Medical Center. It is the first hospital founded in the Texas Medical Center in Houston, Texas. Founded in 1925, it is the primary teaching hospital for McGovern Medical School and the flagship location of 13 hospitals in the Memorial Hermann Healthcare System. It is one of two certified Level I Trauma Centers in the greater Houston area. The Memorial Hermann Life Flight air ambulance service operates its fleet of helicopters from Memorial Hermann–Texas Medical Center. Pediatric care to the hospital is provided by Children's Memorial Hermann Hospital which treats infants, children, teens, and young adults age 0-21.
N. Scott Adzick currently serves as the Surgeon-in-Chief at Children’s Hospital of Philadelphia (CHOP) as well as the Director of CHOP’s Center for Fetal Diagnosis and Treatment, which he founded in 1995. Dr. Adzick is also the C. Everett Koop Professor of Pediatric Surgery at CHOP and a Professor of Pediatrics, Obstetrics and Gynecology at the Perelman School of Medicine at the University of Pennsylvania.

Children's Memorial Hermann Hospital (CMHH) is a nationally ranked women's and pediatric acute care teaching hospital located in Houston, Texas. The hospital has 234 pediatric beds and 76 beds for women. CMHH is affiliated with the John P. and Kathrine G. McGovern Medical School at University of Texas Health Science Center at Houston and is a part of the Memorial Hermann Health System. The hospital provides comprehensive pediatric specialties and subspecialties to infants, children, teens, and young adults aged 0–21 throughout Houston and surrounding regions. Children's Memorial Hermann Hospital also sometimes treats adults that require pediatric care. CMHH also features an American College of Surgeons designated Level 1 Pediatric Trauma Center, 1 of 5 in the state. The hospital is located within the vast Texas Medical Center.
References
- 1 2 Adzick, N. Scott; Thom, Elizabeth A.; Spong, Catherine Y.; Brock, John W.; Burrows, Pamela K.; Johnson, Mark P.; Howell, Lori J.; Farrell, Jody A.; Dabrowiak, Mary E. (2011-03-17). "A randomized trial of prenatal versus postnatal repair of myelomeningocele". The New England Journal of Medicine. 364 (11): 993–1004. doi:10.1056/NEJMoa1014379. ISSN 1533-4406. PMC 3770179 . PMID 21306277.
- ↑ Meuli, M; Meuli-Simmen C; Hutchins GM; et al. "In utero repair of experimental myelomeningocele spares neurologic function at birth". J Pediatr Surg. 196 (31): 397–402.
- ↑ Bouchard, S; Davey MG; Rintoul NE; Walsh DS; Rorke LB; Adzick NS (2003). "Correction of hindbrain herniation and anatomy of the vermis following in utero repair of myelomeningocele in sheep". J Pediatr Surg. 38 (3): 451–58. doi:10.1053/jpsu.2003.50078. PMID 12632366.
- ↑ Pack, PW; Farmer DL; Wilkinson CC; et al. (2000). "Hindbrain herniation develops in surgically created myelomeningocele but is absent after repair in fetal lambs". Obstet Gynecol. 183 (5): 1119–23. doi:10.1067/mob.2000.108867. PMID 11084552.
- ↑ Meuli, M; Meuli-Simmen C; Hutchins GM; et al. (1995). "In utero surgery rescues neurologic function at birth in sheep with spina bifida". Nat Med. 1 (4): 342–47. doi:10.1038/nm0495-342. PMID 7585064. S2CID 29080408.
- ↑ Bruner, J; Tulipan N; Richards W. (1997). "Endoscopic coverage of fetal open myelomeningocele in utero". Am J Obstet Gynecol. 176 (1 Pt 1): 256–57. doi: 10.1016/s0002-9378(97)80050-6 . PMID 9024126.
- ↑ Adzick, N Scott; Sutton, Leslie N; Crombleholme, Timothy M; Flake, Alan W (21 November 1998). "Successful fetal surgery for spina bifida". The Lancet. 352 (9141): 1675–1676. doi: 10.1016/S0140-6736(98)00070-1 . PMID 9853442. S2CID 34483427.
- ↑ Tubbs, RS; Chambers, MR; Smyth, MD; Bartolucci, AA; Bruner, JP; Tulipan, N; Oakes, WJ (March 2003). "Late gestational intrauterine myelomeningocele repair does not improve lower extremity function". Pediatric Neurosurgery. 38 (3): 128–32. doi:10.1159/000068818. PMID 12601237. S2CID 24965555.
- ↑ "Fetal Surgery for Spina Bifida Video". Retrieved on 7 December 2011.
- ↑ Belluck, Pam. "Success of Spina Bifida Study Opens Fetal Surgery Door", "The New York Times", 9 February 2011. Retrieved on 7 December 2011.
- ↑ "Fetal Surgery for Spina Bifida". 2014-03-31.
- ↑ "Facts about Surgery for Myelomeningocele Repair". 2021-04-08.