Bipolar disorder, previously known as manic depression, is a mental disorder characterized by periods of depression and periods of abnormally elevated mood that each last from days to weeks. If the elevated mood is severe or associated with psychosis, it is called mania; if it is less severe, it is called hypomania. During mania, an individual behaves or feels abnormally energetic, happy or irritable, and they often make impulsive decisions with little regard for the consequences. There is usually also a reduced need for sleep during manic phases. During periods of depression, the individual may experience crying and have a negative outlook on life and poor eye contact with others. The risk of suicide is high; over a period of 20 years, 6% of those with bipolar disorder died by suicide, while 30–40% engaged in self-harm. Other mental health issues, such as anxiety disorders and substance use disorders, are commonly associated with bipolar disorder.

Major depressive disorder (MDD), also known as clinical depression, is a mental disorder characterized by at least two weeks of pervasive low mood, low self-esteem, and loss of interest or pleasure in normally enjoyable activities. Introduced by a group of US clinicians in the mid-1970s, the term was adopted by the American Psychiatric Association for this symptom cluster under mood disorders in the 1980 version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), and has become widely used since.
A mental disorder, also referred to as a mental illness, a mental health condition, or a psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. A mental disorder is also characterized by a clinically significant disturbance in an individual's cognition, emotional regulation, or behavior, often in a social context. Such disturbances may occur as single episodes, may be persistent, or may be relapsing–remitting. There are many different types of mental disorders, with signs and symptoms that vary widely between specific disorders. A mental disorder is one aspect of mental health.
Anxiety disorders are a cluster of mental disorders characterized by significant and uncontrollable feelings of anxiety and fear such that a person's social, occupational, and personal functions are significantly impaired. Anxiety may cause physical and cognitive symptoms, such as restlessness, irritability, easy fatigue, difficulty concentrating, increased heart rate, chest pain, abdominal pain, and a variety of other symptoms that may vary based on the individual.

Hypochondriasis or hypochondria is a condition in which a person is excessively and unduly worried about having a serious illness. Hypochondria is an old concept whose meaning has repeatedly changed over its lifespan. It has been claimed that this debilitating condition results from an inaccurate perception of the condition of body or mind despite the absence of an actual medical diagnosis. An individual with hypochondriasis is known as a hypochondriac. Hypochondriacs become unduly alarmed about any physical or psychological symptoms they detect, no matter how minor the symptom may be, and are convinced that they have, or are about to be diagnosed with, a serious illness.

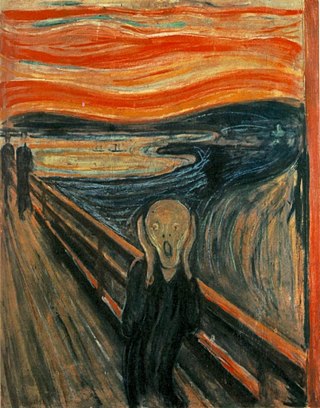
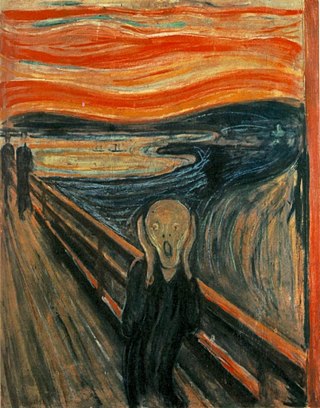
Depression is a mental state of low mood and aversion to activity. It affects more than 280 million people of all ages. Depression affects a person's thoughts, behavior, feelings, and sense of well-being. Depressed people often experience loss of motivation or interest in, or reduced pleasure or joy from, experiences that would normally bring them pleasure or joy. Depressed mood is a symptom of some mood disorders such as major depressive disorder and dysthymia; it is a normal temporary reaction to life events, such as the loss of a loved one; and it is also a symptom of some physical diseases and a side effect of some drugs and medical treatments. It may feature sadness, difficulty in thinking and concentration and a significant increase or decrease in appetite and time spent sleeping. People experiencing depression may have feelings of dejection or hopelessness and may experience suicidal thoughts. It can either be short term or long term.
Adjustment disorder is a maladaptive response to a psychosocial stressor. It is classified as a mental disorder. The maladaptive response usually involves otherwise normal emotional and behavioral reactions that manifest more intensely than usual, causing marked distress, preoccupation with the stressor and its consequences, and functional impairment.

Mental health encompasses emotional, psychological, and social well-being, influencing cognition, perception, and behavior. According to World Health Organization (WHO), it is a "state of well-being in which the individual realizes his or her abilities, can cope with the normal stresses of life, can work productively and fruitfully, and can contribute to his or her community". It likewise determines how an individual handles stress, interpersonal relationships, and decision-making. Mental health includes subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one's intellectual and emotional potential, among others. From the perspectives of positive psychology or holism, mental health may include an individual's ability to enjoy life and to create a balance between life activities and efforts to achieve psychological resilience. Cultural differences, personal philosophy, subjective assessments, and competing professional theories all affect how one defines "mental health". Some early signs related to mental health difficulties are sleep irritation, lack of energy, lack of appetite, thinking of harming oneself or others, self-isolating, and frequently zoning out.
Child psychopathology refers to the scientific study of mental disorders in children and adolescents. Oppositional defiant disorder, attention-deficit hyperactivity disorder, and autism spectrum disorder are examples of psychopathology that are typically first diagnosed during childhood. Mental health providers who work with children and adolescents are informed by research in developmental psychology, clinical child psychology, and family systems. Lists of child and adult mental disorders can be found in the International Statistical Classification of Diseases and Related Health Problems, 10th Edition (ICD-10), published by the World Health Organization (WHO) and in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association (APA). In addition, the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood is used in assessing mental health and developmental disorders in children up to age five.
Suicidal ideation, or suicidal thoughts, is the thought process of having ideas, or ruminations about the possibility of ending one's own life. It is not a diagnosis but is a symptom of some mental disorders, use of certain psychoactive drugs, and can also occur in response to adverse life events without the presence of a mental disorder.
Postpartum blues, also known as baby blues and maternity blues, is a very common but self-limited condition that begins shortly after childbirth and can present with a variety of symptoms such as mood swings, irritability, and tearfulness. Mothers may experience negative mood symptoms mixed with intense periods of joy. Up to 85% of new mothers are affected by postpartum blues, with symptoms starting within a few days after childbirth and lasting up to two weeks in duration. Treatment is supportive, including ensuring adequate sleep and emotional support. If symptoms are severe enough to affect daily functioning or last longer than two weeks, the individual should be evaluated for related postpartum psychiatric conditions, such as postpartum depression and postpartum anxiety. It is unclear whether the condition can be prevented, however education and reassurance are important to help alleviate patient distress.
Child and adolescent psychiatry is a branch of psychiatry that focuses on the diagnosis, treatment, and prevention of mental disorders in children, adolescents, and their families. It investigates the biopsychosocial factors that influence the development and course of psychiatric disorders and treatment responses to various interventions. Child and adolescent psychiatrists primarily use psychotherapy and/or medication to treat mental disorders in the pediatric population.
Dual diagnosis is the condition of having a mental illness and a comorbid substance use disorder. There is considerable debate surrounding the appropriateness of using a single category for a heterogeneous group of individuals with complex needs and a varied range of problems. The concept can be used broadly, for example depression and alcohol use disorder, or it can be restricted to specify severe mental illness and substance use disorder, or a person who has a milder mental illness and a drug dependency, such as panic disorder or generalized anxiety disorder and is dependent on opioids. Diagnosing a primary psychiatric illness in people who use substances is challenging as substance use disorder itself often induces psychiatric symptoms, thus making it necessary to differentiate between substance induced and pre-existing mental illness.
Bipolar II disorder (BP-II) is a mood disorder on the bipolar spectrum, characterized by at least one episode of hypomania and at least one episode of major depression. Diagnosis for BP-II requires that the individual must never have experienced a full manic episode. Otherwise, one manic episode meets the criteria for bipolar I disorder (BP-I).

Major depressive disorder, often simply referred to as depression, is a mental disorder characterized by prolonged unhappiness or irritability. It is accompanied by a constellation of somatic and cognitive signs and symptoms such as fatigue, apathy, sleep problems, loss of appetite, loss of engagement, low self-regard/worthlessness, difficulty concentrating or indecisiveness, or recurrent thoughts of death or suicide.

Mental health in education is the impact that mental health has on educational performance. Mental health often viewed as an adult issue, but in fact, almost half of adolescents in the United States are affected by mental disorders, and about 20% of these are categorized as “severe.” Mental health issues can pose a huge problem for students in terms of academic and social success in school. Education systems around the world treat this topic differently, both directly through official policies and indirectly through cultural views on mental health and well-being. These curriculums are in place to effectively identify mental health disorders and treat it using therapy, medication, or other tools of alleviation.
In colleges and universities in the United States, suicide is one of the most common causes of death among students. Each year, approximately 24,000 college students attempt suicide while 1,100 students succeed in their attempt, making suicide the second-leading cause of death among U.S. college students. Roughly 12% of college students report the occurrence of suicide ideation during their first four years in college, with 2.6% percent reporting persistent suicide ideation. 65% of college students reported that they knew someone who has either attempted or died by suicide, showing that the majority of students on college campuses are exposed to suicide or suicidal attempts.

Mental health issues are prevalent in South Korea, with the highest suicide rate in the OECD and the highest rate of hospitalizations for mental illness among OECD countries. South Korea has state-funded mental health services, the majority of which are inpatient hospital facilities, but they are largely underfunded and underutilized. Despite the prevalence of mental illness, social stigma remains prevalent throughout the South Korean population, which discourages sufferers from seeking treatment. Mental illness, while present across all demographic groups, is most common among the elderly and adolescents in South Korea.

The COVID-19 pandemic has impacted the mental health of people across the globe. The pandemic has caused widespread anxiety, depression, and post-traumatic stress disorder symptoms. According to the UN health agency WHO, in the first year of the COVID-19 pandemic, prevalence of common mental health conditions, such as depression and anxiety, went up by more than 25 percent. The pandemic has damaged social relationships, trust in institutions and in other people, has caused changes in work and income, and has imposed a substantial burden of anxiety and worry on the population. Women and young people face the greatest risk of depression and anxiety.

A systematic review notes that children with COVID-19 have milder effects and better prognoses than adults. However, children are susceptible to "multisystem inflammatory syndrome in children" (MIS-C), a rare but life-threatening systemic illness involving persistent fever and extreme inflammation following exposure to the SARS-CoV-2 virus.