Related Research Articles

Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. These may occur a few times a day or a few times per week. Depending on the person, asthma symptoms may become worse at night or with exercise.

In organic chemistry, isocyanate is the functional group with the formula R−N=C=O. Organic compounds that contain an isocyanate group are referred to as isocyanates. An organic compound with two isocyanate groups is known as a diisocyanate. Diisocyanates are manufactured for the production of polyurethanes, a class of polymers.

A cough is a sudden expulsion of air through the large breathing passages which can help clear them of fluids, irritants, foreign particles and microbes. As a protective reflex, coughing can be repetitive with the cough reflex following three phases: an inhalation, a forced exhalation against a closed glottis, and a violent release of air from the lungs following opening of the glottis, usually accompanied by a distinctive sound.

Rhinitis, also known as coryza, is irritation and inflammation of the mucous membrane inside the nose. Common symptoms are a stuffy nose, runny nose, sneezing, and post-nasal drip.

Hypersensitivity pneumonitis (HP) or extrinsic allergic alveolitis (EAA) is a syndrome caused by the repetitive inhalation of antigens from the environment in susceptible or sensitized people. Common antigens include molds, bacteria, bird droppings, bird feathers, agricultural dusts, bioaerosols and chemicals from paints or plastics. People affected by this type of lung inflammation (pneumonitis) are commonly exposed to the antigens by their occupations, hobbies, the environment and animals. The inhaled antigens produce a hypersensitivity immune reaction causing inflammation of the airspaces (alveoli) and small airways (bronchioles) within the lung. Hypersensitivity pneumonitis may eventually lead to interstitial lung disease.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.

Byssinosis is an occupational lung disease caused by inhalation of cotton or jute dust in inadequately ventilated working environments and can develop over time with repeated exposure. Byssinosis commonly occurs in textile workers who are employed in yarn and fabric manufacture industries. It is now thought that the cotton dust directly causes the disease and some believe that the causative agents are endotoxins that come from the cell walls of gram-negative bacteria that grow on the cotton. Although bacterial endotoxin is a likely cause, the absence of similar symptoms in workers in other industries exposed to endotoxins makes this uncertain. Current smokers are also at risk for developing byssinosis or having complications relating to byssinosis.
Exercise-induced bronchoconstriction (EIB) occurs when the airways narrow as a result of exercise. This condition has been referred to as exercise-induced asthma (EIA); however, this term is no longer preferred. While exercise does not cause asthma, it is frequently an asthma trigger.
Occupational lung diseases comprise a broad group of diseases, including occupational asthma, industrial bronchitis, chronic obstructive pulmonary disease (COPD), bronchiolitis obliterans, inhalation injury, interstitial lung diseases, infections, lung cancer and mesothelioma. These can be caused directly or due to immunological response to an exposure to a variety of dusts, chemicals, proteins or organisms. Occupational cases of interstitial lung disease may be misdiagnosed as COPD, idiopathic pulmonary fibrosis, or a myriad of other diseases; leading to a delay in identification of the causative agent.
Reactive airway disease (RAD) is an informal label that physicians apply to patients with symptoms similar to those of asthma. An exact definition of the condition does not exist. Individuals who are typically labeled as having RAD generally have a history of wheezing, coughing, dyspnea, and production of sputum that may or may not be caused by asthma. Symptoms may also include, but are not limited to, coughing, shortness of breath, excess mucus in the bronchial tube, swollen mucous membrane in the bronchial tube, and/or hypersensitive bronchial tubes. Physicians most commonly label patients with RAD when they are hesitant about formally diagnosing a patient with asthma, which is most prevalent in the pediatric setting. While some physicians may use RAD and asthma synonymously, there is controversy over this usage.
The use of podiatry drills, in the absence of engineering controls and personal protective equipment, is an occupational hazard to the healthcare provider. Nail dust collected during foot care procedures performed in office settings has been found to contain keratin, keratin hydrolysates, microbial debris, and viable fungal elements, including dermatophytes and saprotrophs. Exposure to nail dust and the associated risk will vary with the policies and practices in place, the type of podiatry drill used, therapy technique, frequency of procedures, personal protective equipment utilized and the use of ventilation systems.
The specific inhalation challenge (SIC) is a diagnosis tool to assess airway responsiveness to "sensitizing" substances as opposed to nonspecific stimuli such as pharmacological agents, cold air and exercise. Subjects are exposed to a suspected occupational agent in a controlled way under close supervision in a hospital laboratory. The specific inhalation challenges has been considered as the gold standard in confirming the diagnosis of occupational asthma.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.
Vocal cord dysfunction (VCD) is a pathology affecting the vocal folds characterized by full or partial vocal fold closure causing difficulty and distress during respiration, especially during inhalation.

In medicine, exhaled nitric oxide (eNO) can be measured in a breath test for asthma and other respiratory conditions characterized by airway inflammation. Nitric oxide (NO) is a gaseous molecule produced by certain cell types in an inflammatory response. The fraction of exhaled NO (FENO) is a promising biomarker for the diagnosis, follow-up and as a guide to therapy in adults and children with asthma. The breath test has recently become available in many well-equipped hospitals in developed countries, although its exact role remains unclear.
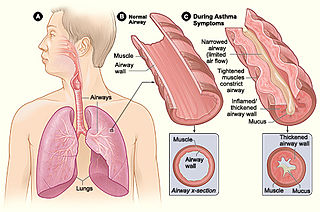
Asthma is a common pulmonary condition defined by chronic inflammation of respiratory tubes, tightening of respiratory smooth muscle, and episodes of bronchoconstriction. The Centers for Disease Control and Prevention estimate that 1 in 11 children and 1 in 12 adults have asthma in the United States of America. According to the World Health Organization, asthma affects 235 million people worldwide. There are two major categories of asthma: allergic and non-allergic. The focus of this article will be allergic asthma. In both cases, bronchoconstriction is prominent.
Acute inhalation injury may result from frequent and widespread use of household cleaning agents and industrial gases. The airways and lungs receive continuous first-pass exposure to non-toxic and irritant or toxic gases via inhalation. Irritant gases are those that, on inhalation, dissolve in the water of the respiratory tract mucosa and provoke an inflammatory response, usually from the release of acidic or alkaline radicals. Smoke, chlorine, phosgene, sulfur dioxide, hydrogen chloride, hydrogen sulfide, nitrogen dioxide, ozone, and ammonia are common irritants.

Flock worker's lung is an occupational lung disease caused by exposure to flock, small fibers that are glued to a backing in order to create a specific texture. People who work in flocking are at risk of inhaling small pieces of the flock fibers, which causes interstitial lung disease. The disease was initially described in 1998, when a group of workers at a flocking plant developed interstitial lung disease of unknown cause.
Chronic cough is long-term coughing, sometimes defined as more than several weeks or months. Generally a cough lasting for more than eight weeks for an adult would meet the clinical definition of a chronic cough; and for children this threshold is lower. The term can be used to describe the different causes related to coughing, the three main ones being upper airway cough syndrome, asthma and gastroesophageal reflux disease. It occurs in the upper airway of the respiratory system. Generally, a cough lasts around one to two weeks; however, chronic cough can persist for an extended period of time defined as six weeks or longer. People with chronic cough often experience more than one cause present. Due to the nature of the syndrome, the treatments used are similar; however, there are a subsequent number of treatments available, and the clinical management of the patients remains a challenge. Risk factors include exposure to cigarette smoke, and exposure to pollution, especially particulates.
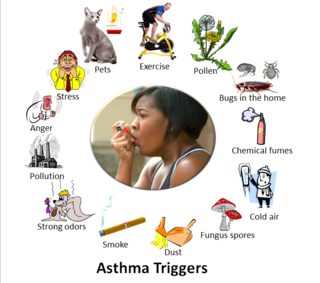
Asthma triggers are factors or stimuli that provoke the exacerbation of asthma symptoms or increase the degree of airflow disruption, which can lead to an asthma attack. An asthma attack is characterized by an obstruction of the airway, hypersecretion of mucus and bronchoconstriction due to the contraction of smooth muscles around the respiratory tract. Its symptoms include a wide range of manifestations such as breathlessness, coughing, a tight chest and wheezing.
References
- 1 2 3 4 Tarlo, Susan M.; Balmes, John; Balkissoon, Ronald; Beach, Jeremy; Beckett, William; Bernstein, David; Blanc, Paul D.; Brooks, Stuart M.; Cowl, Clayton T. (September 2008). "Diagnosis and management of work-related asthma: American College Of Chest Physicians Consensus Statement". Chest. 134 (3 Suppl): 1S–41S. doi:10.1378/chest.08-0201. ISSN 0012-3692. PMID 18779187.
- 1 2 3 Murray & Nadel's Textbook of Respiratory Medicine. Elsevier. 2016. pp. 1295–1306. ISBN 9781455733835.
- 1 2 3 4 Tarlo, Susan M.; Lemiere, Catherine (2014-02-13). "Occupational asthma". The New England Journal of Medicine. 370 (7): 640–649. doi:10.1056/NEJMra1301758. ISSN 1533-4406. PMID 24521110.
- 1 2 Henneberger, Paul K.; Redlich, Carrie A.; Callahan, David B.; Harber, Philip; Lemière, Catherine; Martin, James; Tarlo, Susan M.; Vandenplas, Olivier; Torén, Kjell (2011-08-01). "An official american thoracic society statement: work-exacerbated asthma". American Journal of Respiratory and Critical Care Medicine. 184 (3): 368–378. doi:10.1164/rccm.812011ST. ISSN 1535-4970. PMID 21804122.
- ↑ "Asthma & Allergies". NIOSH. April 3, 2012.
- ↑ (T78) Occupational Asthma : Table of agents, products and substances which can cause asthma
- ↑ Baur, Xaver; Bakehe, Prudence (May 2014). "Allergens causing occupational asthma: an evidence-based evaluation of the literature". International Archives of Occupational and Environmental Health. 87 (4): 339–363. doi:10.1007/s00420-013-0866-9. ISSN 1432-1246. PMID 23595938. S2CID 38640302.
- 1 2 de Groene, Gerda J.; Pal, Teake M.; Beach, Jeremy; Tarlo, Susan M.; Spreeuwers, Dick; Frings-Dresen, Monique Hw; Mattioli, Stefano; Verbeek, Jos H. (2011). "Workplace interventions for treatment of occupational asthma". The Cochrane Database of Systematic Reviews (5): CD006308. doi:10.1002/14651858.CD006308.pub3. ISSN 1469-493X. PMID 21563151.
- ↑ Ameille J, Pauli G, Calastreng-Crinquand A, et al. (February 2003). "Reported incidence of occupational asthma in France, 1996–99: the ONAP programme". Occup Environ Med. 60 (2): 136–41. doi:10.1136/oem.60.2.136. PMC 1740458 . PMID 12554842.
- 1 2 Chan-Yeung, Moira; Malo, Jean-Luc (1995). "Occupational Asthma". New England Journal of Medicine. 333 (2): 107–112. doi:10.1056/NEJM199507133330207. ISSN 0028-4793. PMID 7777015.
- ↑ "Occupational asthma". Mayo Clinic. 23 May 2009.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "OSH Answers Asthma, Work-related". Canadian Centre for Occupational Health and Safety. December 16, 2013.
- 1 2 3 Baur, X.; Sigsgaard, T.; Aasen, T. B.; Burge, P. S.; Heederik, D.; Henneberger, P.; Maestrelli, P.; Rooyackers, J.; Schlünssen, V. (2012-03-01). "Guidelines for the management of work-related asthma". European Respiratory Journal. 39 (3): 529–545. doi: 10.1183/09031936.00096111 . ISSN 0903-1936. PMID 22379148.
- 1 2 "Occupational/Work-Related Asthma Medical Treatment Guideline" (PDF).
- ↑ Moscato, G.; Godnic-Cvar, J.; Maestrelli, P.; Malo, J. L.; Burge, P. S.; Coifman, R. (September 1995). "Statement on self-monitoring of peak expiratory flows in the investigation of occupational asthma. Subcommittee on Occupational Allergy of the European Academy of Allergology and Clinical Immunology. American Academy of Allergy and Clinical Immunology. European Respiratory Society. American College of Allergy, Asthma and Immunology". The European Respiratory Journal. 8 (9): 1605–1610. doi: 10.1183/09031936.95.08091605 . ISSN 0903-1936. PMID 8575590.
- ↑ Vandenplas, Olivier; Suojalehto, Hille; Aasen, Tor B.; Baur, Xaver; Burge, P. Sherwood; de Blay, Frederic; Fishwick, David; Hoyle, Jennifer; Maestrelli, Piero (June 2014). "Specific inhalation challenge in the diagnosis of occupational asthma: consensus statement". The European Respiratory Journal. 43 (6): 1573–1587. doi: 10.1183/09031936.00180313 . ISSN 1399-3003. PMID 24603815.
- ↑ Tarlo, Susan M.; Liss, Gary M. (July 2010). "Prevention of occupational asthma". Current Allergy and Asthma Reports. 10 (4): 278–286. doi:10.1007/s11882-010-0118-y. ISSN 1534-6315. PMID 20424999. S2CID 20166471.
- ↑ "NIOSH: Prevention of Work-related Asthma". 2018-11-23.
- 1 2 Henneberger, Paul K; Patel, Jenil R; de Groene, Gerda J; Beach, Jeremy; Tarlo, Susan M; Pal, Teake M; Curti, Stefania (2019-10-08). Cochrane Work Group (ed.). "Workplace interventions for treatment of occupational asthma". Cochrane Database of Systematic Reviews. 10 (10): CD006308. doi:10.1002/14651858.CD006308.pub4. PMC 6781842 . PMID 31593318.
- 1 2 "NIOSH: Work-related asthma". 2019-01-03.
- 1 2 Cowl, Clayton T. (2011). "Occupational Asthma". Chest. 139 (3): 674–681. doi:10.1378/chest.10-0079. PMID 21362654.
- ↑ "Occuptational Asthma". MedlinePlus Medical Encyclopedia.
- ↑ Dewitte JD, Chan-Yeung M, Malo JL (May 1994). "Medicolegal and compensation aspects of occupational asthma". Eur. Respir. J. 7 (5): 969–80. doi: 10.1183/09031936.94.07050969 . PMID 8050556. S2CID 41120422.
- ↑ Leigh JP, Romano PS, Schenker MB, Kreiss K (January 2002). "Costs of occupational COPD and asthma". Chest. 121 (1): 264–72. CiteSeerX 10.1.1.455.4942 . doi:10.1378/chest.121.1.264. PMID 11796461.