Amenorrhea is the absence of a menstrual period in a female who has reached reproductive age. Physiological states of amenorrhoea are seen, most commonly, during pregnancy and lactation (breastfeeding). Outside the reproductive years, there is absence of menses during childhood and after menopause.

Hyperprolactinaemia is the presence of abnormally high levels of prolactin in the blood. Normal levels average to about 13 ng/mL in women, and 5 ng/mL in men, with an upper normal limit of serum prolactin levels being 15–25 ng/mL for both. When the fasting levels of prolactin in blood exceed this upper limit, hyperprolactinemia is indicated.
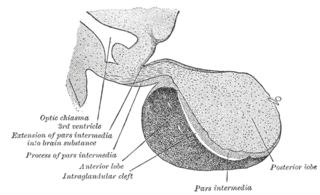
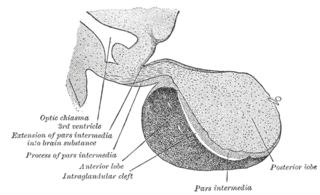
A major organ of the endocrine system, the anterior pituitary is the glandular, anterior lobe that together with the posterior lobe makes up the pituitary gland (hypophysis) which, in humans, is located at the base of the brain, protruding off the bottom of the hypothalamus.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal glands—also referred to as the adrenal cortex—normally secrete glucocorticoids, mineralocorticoids, and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes to organ failure and shock. Adrenal crisis may occur if a person having adrenal insufficiency experiences stresses, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow.
Corticotropes are basophilic cells in the anterior pituitary that produce pro-opiomelanocortin (POMC) which undergoes cleavage to adrenocorticotropin (ACTH), β-lipotropin (β-LPH), and melanocyte-stimulating hormone (MSH). These cells are stimulated by corticotropin releasing hormone (CRH) and make up 15–20% of the cells in the anterior pituitary. The release of ACTH from the corticotropic cells is controlled by CRH, which is formed in the cell bodies of parvocellular neurosecretory cells within the paraventricular nucleus of the hypothalamus and passes to the corticotropes in the anterior pituitary via the hypophyseal portal system. Adrenocorticotropin hormone stimulates the adrenal cortex to release glucocorticoids and plays an important role in the stress response.
Delayed puberty is when a person lacks or has incomplete development of specific sexual characteristics past the usual age of onset of puberty. The person may have no physical or hormonal signs that puberty has begun. In the United States, girls are considered to have delayed puberty if they lack breast development by age 13 or have not started menstruating by age 15. Boys are considered to have delayed puberty if they lack enlargement of the testicles by age 14. Delayed puberty affects about 2% of adolescents.
Congenital adrenal hyperplasia due to 17α-hydroxylase deficiency is an uncommon form of congenital adrenal hyperplasia (CAH) resulting from a mutation in the gene CYP17A1, which produces the enzyme 17α-hydroxylase. It causes decreased synthesis of cortisol and sex hormones, with resulting increase in mineralocorticoid production. Thus, common symptoms include mild cortisol deficiency, ambiguous genitalia in men or amenorrhea at puberty in women, and hypokalemic hypertension. However, partial (incomplete) deficiency often has inconsistent symptoms between patients, and affected women may be asymptomatic except for infertility.
Hypogonadism means diminished functional activity of the gonads—the testicles or the ovaries—that may result in diminished production of sex hormones. Low androgen levels are referred to as hypoandrogenism and low estrogen as hypoestrogenism. These are responsible for the observed signs and symptoms in both males and females.
Gonadarche refers to the earliest gonadal changes of puberty. In response to pituitary gonadotropins, the ovaries in females and the testes in males begin to grow and increase the production of the sex steroids, especially estradiol and testosterone. The ovary and testis have receptors, follicle cells and leydig cells, respectively, where gonadotropins bind to stimulate the maturation of the gonads and secretion of estrogen and testosterone. Certain disorders can result in changes to timing or nature of these processes.
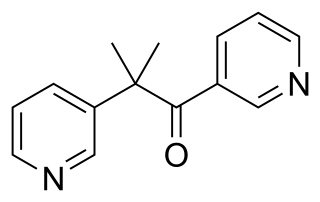
Metyrapone, sold under the brand name Metopirone, is a medication which is used in the diagnosis of adrenal insufficiency and occasionally in the treatment of Cushing's syndrome (hypercortisolism). It is part of the steroidogenesis inhibitor class of drugs.
Kallmann syndrome (KS) is a genetic disorder that prevents a person from starting or fully completing puberty. Kallmann syndrome is a form of a group of conditions termed hypogonadotropic hypogonadism. To distinguish it from other forms of hypogonadotropic hypogonadism, Kallmann syndrome has the additional symptom of a total lack of sense of smell (anosmia) or a reduced sense of smell. If left untreated, people will have poorly defined secondary sexual characteristics, show signs of hypogonadism, almost invariably are infertile and are at increased risk of developing osteoporosis. A range of other physical symptoms affecting the face, hands and skeletal system can also occur.

A gonadotropin-releasing hormone agonist is a type of medication which affects gonadotropins and sex hormones. They are used for a variety of indications including in fertility medicine and to lower sex hormone levels in the treatment of hormone-sensitive cancers such as prostate cancer and breast cancer, certain gynecological disorders like heavy periods and endometriosis, high testosterone levels in women, early puberty in children, as a part of transgender hormone therapy, and to delay puberty in transgender youth among other uses. It is also used in the suppression of spontaneous ovulation as part of controlled ovarian hyperstimulation, an essential component in IVF. GnRH agonists are given by injections into fat, as implants placed into fat, and as nasal sprays.
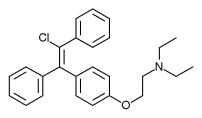
Enclomifene (INNTooltip International Nonproprietary Name), or enclomiphene (USANTooltip United States Adopted Name), a nonsteroidal selective estrogen receptor modulator of the triphenylethylene group acts by antagonizing the estrogen receptor (ER) in the pituitary gland, which reduces negative feedback by estrogen on the hypothalamic-pituitary-gonadal axis, thereby increasing gonadotropin secretion and hence gonadal production of testosterone. It is one of the two stereoisomers of clomifene, which itself is a mixture of 38% zuclomifene and 62% enclomifene. Enclomifene is the (E)-stereoisomer of clomifene, while zuclomifene is the (Z)-stereoisomer. Whereas zuclomifene is more estrogenic, enclomifene is more antiestrogenic. In accordance, unlike enclomifene, zuclomifene is antigonadotropic due to activation of the ER and reduces testosterone levels in men. As such, isomerically pure enclomifene is more favorable than clomifene as a progonadotropin for the treatment of male hypogonadism.
Functional hypothalamic amenorrhea (FHA) is a form of amenorrhea and chronic anovulation and is one of the most common types of secondary amenorrhea. It is classified as hypogonadotropic hypogonadism. It was previously known as "juvenile hypothalamosis syndrome," prior to the discovery that sexually mature females are equally affected. FHA has multiple risk factors, with links to stress-related, weight-related, and exercise-related factors. FHA is caused by stress-induced suppression of the hypothalamic-pituitary-ovarian (HPO) axis, which results in inhibition of gonadotropin-releasing hormone (GnRH) secretion, and gonadotropins, follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Severe and potentially prolonged hypoestrogenism is perhaps the most dangerous hormonal pathology associated with the disease, because consequences of this disturbance can influence bone health, cardiovascular health, mental health, and metabolic functioning in both the short and long-term. Because many of the symptoms overlap with those of organic hypothalamic, pituitary, or gonadal disease and therefore must be ruled out, FHA is a diagnosis of exclusion; "functional" is used to indicate a behavioral cause, in which no anatomical or organic disease is identified, and is reversible with correction of the underlying cause. Diagnostic workup includes a detailed history and physical, laboratory studies, such as a pregnancy test, and serum levels of FSH and LH, prolactin, and thyroid-stimulating hormone (TSH), and imaging. Additional tests may be indicated in order to distinguish FHA from organic hypothalamic or pituitary disorders. Patients present with a broad range of symptoms related to severe hypoestrogenism as well as hypercortisolemia, low serum insulin levels, low serum insulin-like growth factor 1 (IGF-1), and low total triiodothyronine (T3). Treatment is primarily managing the primary cause of the FHA with behavioral modifications. While hormonal-based therapies are potential treatment to restore menses, weight gain and behavioral modifications can have an even more potent impact on reversing neuroendocrine abnormalities, preventing further bone loss, and re-establishing menses, making this the recommended line of treatment. If this fails to work, secondary treatment is aimed at treating the effects of hypoestrogenism, hypercortisolism, and hypothyroidism.
Autoimmune hypophysitis is defined as inflammation of the pituitary gland due to autoimmunity.
Hypergonadotropic hypogonadism (HH), also known as primary or peripheral/gonadal hypogonadism or primary gonadal failure, is a condition which is characterized by hypogonadism which is due to an impaired response of the gonads to the gonadotropins, follicle-stimulating hormone (FSH) and luteinizing hormone (LH), and in turn a lack of sex steroid production. As compensation and the lack of negative feedback, gonadotropin levels are elevated. Individuals with HH have an intact and functioning hypothalamus and pituitary glands so they are still able to produce FSH and LH. HH may present as either congenital or acquired, but the majority of cases are of the former nature. HH can be treated with hormone replacement therapy.
An antigonadotropin is a drug which suppresses the activity and/or downstream effects of one or both of the gonadotropins, follicle-stimulating hormone (FSH) and luteinizing hormone (LH). This results in an inhibition of the hypothalamic-pituitary-gonadal (HPG) axis, and thus a decrease in the levels of the androgen, estrogen, and progestogen sex steroids in the body. Antigonadotropins also inhibit ovulation in women and spermatogenesis in men. They are used for a variety of purposes, including for the hormonal birth control, treatment of hormonally-sensitive cancers, to delay precocious puberty and puberty in transgender youth, as a form of chemical castration to reduce the sex drives of individuals with hypersexuality or pedophilia, and to treat estrogen-associated conditions in women such as menorrhagia and endometriosis, among others. High-dose antigonadotropin therapy has been referred to as medical castration.
Gonadotropin-releasing hormone (GnRH) insensitivity also known as Isolated gonadotropin-releasing hormone (GnRH)deficiency (IGD) is a rare autosomal recessive genetic and endocrine syndrome which is characterized by inactivating mutations of the gonadotropin-releasing hormone receptor (GnRHR) and thus an insensitivity of the receptor to gonadotropin-releasing hormone (GnRH), resulting in a partial or complete loss of the ability of the gonads to synthesize the sex hormones. The condition manifests itself as isolated hypogonadotropic hypogonadism (IHH), presenting with symptoms such as delayed, reduced, or absent puberty, low or complete lack of libido, and infertility, and is the predominant cause of IHH when it does not present alongside anosmia.
Hypogonadotropic hypogonadism (HH), is due to problems with either the hypothalamus or pituitary gland affecting the hypothalamic-pituitary-gonadal axis. Hypothalamic disorders result from a deficiency in the release of gonadotropic releasing hormone (GnRH), while pituitary gland disorders are due to a deficiency in the release of gonadotropins from the anterior pituitary. GnRH is the central regulator in reproductive function and sexual development via the HPG axis. GnRH is released by GnRH neurons, which are hypothalamic neuroendocrine cells, into the hypophyseal portal system acting on gonadotrophs in the anterior pituitary. The release of gonadotropins, LH and FSH, act on the gonads for the development and maintenance of proper adult reproductive physiology. LH acts on Leydig cells in the male testes and theca cells in the female. FSH acts on Sertoli cells in the male and follicular cells in the female. Combined this causes the secretion of gonadal sex steroids and the initiation of folliculogenesis and spermatogenesis. The production of sex steroids forms a negative feedback loop acting on both the anterior pituitary and hypothalamus causing a pulsatile secretion of GnRH. GnRH neurons lack sex steroid receptors and mediators such as kisspeptin stimulate GnRH neurons for pulsatile secretion of GnRH.

The side effects of radiotherapy on fertility are a growing concern to patients undergoing radiotherapy as cancer treatments. Radiotherapy is essential for certain cancer treatments and often is the first point of call for patients. Radiation can be divided into two categories: ionising radiation (IR) and non-ionising radiation (NIR). IR is more dangerous than NIR and a source of this radiation is X-rays used in medical procedures, for example in radiotherapy.