The National Institute of Allergy and Infectious Diseases is one of the 27 institutes and centers that make up the National Institutes of Health (NIH), an agency of the United States Department of Health and Human Services (HHS). NIAID's mission is to conduct basic and applied research to better understand, treat, and prevent infectious, immunologic, and allergic diseases.

Neisseria meningitidis, often referred to as meningococcus, is a Gram-negative bacterium that can cause meningitis and other forms of meningococcal disease such as meningococcemia, a life-threatening sepsis. The bacterium is referred to as a coccus because it is round, and more specifically a diplococcus because of its tendency to form pairs.

Meningococcal disease describes infections caused by the bacterium Neisseria meningitidis. It has a high mortality rate if untreated but is vaccine-preventable. While best known as a cause of meningitis, it can also result in sepsis, which is an even more damaging and dangerous condition. Meningitis and meningococcemia are major causes of illness, death, and disability in both developed and under-developed countries.
The Joint Committee on Vaccination and Immunisation (JCVI) is an independent expert advisory committee that advises United Kingdom health departments on immunisation, making recommendations concerning vaccination schedules and vaccine safety. It has a statutory role in England and Wales, and health departments in Scotland and Northern Ireland may choose to accept its advice.
The Haemophilus influenzae type B vaccine, also known as Hib vaccine, is a vaccine used to prevent Haemophilus influenzae type b (Hib) infection. In countries that include it as a routine vaccine, rates of severe Hib infections have decreased more than 90%. It has therefore resulted in a decrease in the rate of meningitis, pneumonia, and epiglottitis.
John Bennett Robbins was a senior investigator at the National Institutes of Health (NIH), best known for his contribution to the development of the vaccine against bacterial meningitis with his colleague Rachel Schneerson. He conducted research on the Bethesda, Maryland campus of the NIH from 1970 until his retirement at the age of 80 in 2012. During his tenure, he worked in the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Food and Drug Administration’s biologics laboratories on location.

JN-International Medical Corporation (JNIMC) is a U.S.-based biopharmaceutical corporation which since 1998 has been focused on developing vaccines and diagnostics for infectious disease for developing countries. This private corporation was founded in 1998 by Dr. Jeeri R. Reddy with the help of Dr. Kelly F. Lechtenberg in a small rural town, Oakland, Nebraska. From there it grew and expanded until in the year 2000 the corporation moved to Omaha, Nebraska.
NmVac4-A/C/Y/W-135 is the commercial name of the polysaccharide vaccine against the bacterium that causes meningococcal meningitis. The product, by JN-International Medical Corporation, is designed and formulated to be used in developing countries for protecting populations during meningitis disease epidemics.

Meningitis is acute or chronic inflammation of the protective membranes covering the brain and spinal cord, collectively called the meninges. The most common symptoms are fever, headache, and neck stiffness. Other symptoms include confusion or altered consciousness, nausea, vomiting, and an inability to tolerate light or loud noises. Young children often exhibit only nonspecific symptoms, such as irritability, drowsiness, or poor feeding. A non-blanching rash may also be present.
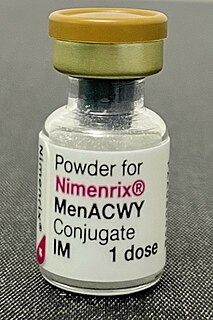
Meningococcal vaccine refers to any vaccine used to prevent infection by Neisseria meningitidis. Different versions are effective against some or all of the following types of meningococcus: A, B, C, W-135, and Y. The vaccines are between 85 and 100% effective for at least two years. They result in a decrease in meningitis and sepsis among populations where they are widely used. They are given either by injection into a muscle or just under the skin.
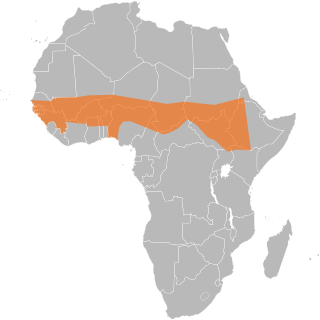
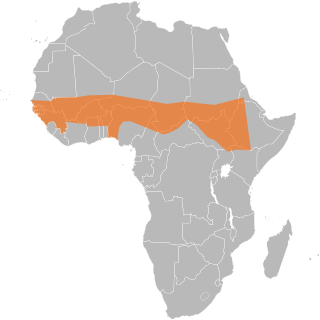
The African meningitis belt is a region in sub-Saharan Africa where the rate of incidence of meningitis is very high. It extends from Senegal to Ethiopia, and the primary cause of meningitis in the belt is Neisseria meningitidis.
MenAfriVac is a vaccine developed for use in sub-Saharan Africa for children and adults between 9 months and 29 years of age against meningococcal bacterium Neisseria meningitidis group A. The vaccine costs less than US$0.50 per dose.
The Vaccine Damage Payment is a provision of the welfare state in the United Kingdom that provides a substantial payment for people who can show that they have suffered a vaccine injury.
Noni E. MacDonald is a Canadian physician. She is a Professor in the Department of Pediatrics and former Dean of the Faculty of Medicine at Dalhousie University. In 2019, MacDonald was awarded the Order of Nova Scotia and Order of Canada.
Sir Andrew John Pollard is a Professor of Paediatric Infection and Immunity at the University of Oxford and a Fellow of St Cross College, Oxford. He is an Honorary Consultant Paediatrician at John Radcliffe Hospital and the Director of the Oxford Vaccine Group. He is the Chief Investigator on the University of Oxford COVID-19 Vaccine trials and has led research on vaccines for many life-threatening infectious diseases including typhoid fever, Neisseria meningitidis, Haemophilus influenzae type b, streptococcus pneumoniae, pertussis, influenza, rabies, and Ebola.
Helen Aspasia Petousis-Harris is a New Zealand vaccinologist and associate professor in the Department of General Practice and Primary Health Care at the University of Auckland. She has been involved in research related to vaccination in New Zealand since 1998, with her main areas of focus being vaccine safety and effectiveness. Petousis-Harris has had a variety of lead roles in New Zealand and international organisations that focus on vaccination and is a regular media spokesperson in this field, especially during the COVID-19 pandemic.
Maheshi N. Ramasamy is a British-Sri Lankan physician and lecturer. She is currently working as one of the chief investigators at the Oxford Vaccine Group.

Shabir Ahmed Madhi is a South African physician who is professor of vaccinology and director of the South African Medical Research Council Respiratory and Meningeal Pathogens Research Unit at the University of the Witwatersrand, and National Research Foundation/Department of Science and Technology Research Chair in Vaccine Preventable Diseases. In January 2021, he was appointed Dean of the Faculty of Health Sciences at the University of the Witwateratand.

Immunisation against infectious disease, popularly known as The Green Book, provides information on vaccines for vaccine-preventable diseases. It acts as a guide to the UK's vaccination schedule for health professionals and health departments that give vaccines in the United Kingdom.
Helen Siobhan Marshall is an Australian medical researcher who is Professor of Vaccinology at the University of Adelaide. She was named the South Australian of the Year for 2022.