Related Research Articles
A hallucination is a perception in the absence of an external stimulus that has the qualities of a real perception. Hallucinations are vivid, substantial, and are perceived to be located in external objective space. Hallucination is a combination of two conscious states of brain wakefulness and REM sleep. They are distinguishable from several related phenomena, such as dreaming, which does not involve wakefulness; pseudohallucination, which does not mimic real perception, and is accurately perceived as unreal; illusion, which involves distorted or misinterpreted real perception; and mental imagery, which does not mimic real perception, and is under voluntary control. Hallucinations also differ from "delusional perceptions", in which a correctly sensed and interpreted stimulus is given some additional significance.

In visual perception, an optical illusion is an illusion caused by the visual system and characterized by a visual percept that arguably appears to differ from reality. Illusions come in a wide variety; their categorization is difficult because the underlying cause is often not clear but a classification proposed by Richard Gregory is useful as an orientation. According to that, there are three main classes: physical, physiological, and cognitive illusions, and in each class there are four kinds: Ambiguities, distortions, paradoxes, and fictions. A classical example for a physical distortion would be the apparent bending of a stick half immerged in water; an example for a physiological paradox is the motion aftereffect. An example for a physiological fiction is an afterimage. Three typical cognitive distortions are the Ponzo, Poggendorff, and Müller-Lyer illusion. Physical illusions are caused by the physical environment, e.g. by the optical properties of water. Physiological illusions arise in the eye or the visual pathway, e.g. from the effects of excessive stimulation of a specific receptor type. Cognitive visual illusions are the result of unconscious inferences and are perhaps those most widely known.

Micropsia is a condition affecting human visual perception in which objects are perceived to be smaller than they actually are. Micropsia can be caused by optical factors, by distortion of images in the eye, by changes in the brain, and from psychological factors. Dissociative phenomena are linked with micropsia, which may be the result of brain-lateralization disturbance.

Alice in Wonderland syndrome (AIWS), also known as Todd's syndrome or dysmetropsia, is a neurological disorder that distorts perception. People with this syndrome may experience distortions in their visual perception of objects, such as appearing smaller (micropsia) or larger (macropsia), or appearing to be closer (pelopsia) or farther (teleopsia) than they are. Distortion may also occur for senses other than vision.

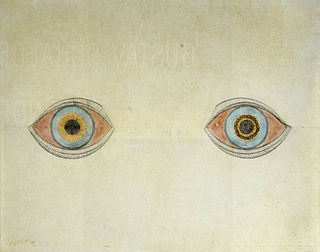
An afterimage is an image that continues to appear in the eyes after a period of exposure to the original image. An afterimage may be a normal phenomenon or may be pathological (palinopsia). Illusory palinopsia may be a pathological exaggeration of physiological afterimages. Afterimages occur because photochemical activity in the retina continues even when the eyes are no longer experiencing the original stimulus.
Visual release hallucinations, also known as Charles Bonnet syndrome or CBS, are a type of psychophysical visual disturbance in which a person with partial or severe blindness experiences visual hallucinations.
Visual snow syndrome (VSS) is an uncommon neurological condition in which the primary symptom is that affected individuals see persistent flickering white, black, transparent, or coloured dots across the whole visual field.
Hallucinogen persisting perception disorder (HPPD) is a non-psychotic disorder in which a person experiences apparent lasting or persistent visual hallucinations or perceptual distortions after using drugs, including but not limited to psychedelics, dissociatives, entactogens, tetrahydrocannabinol (THC), and SSRIs. Despite being designated as a hallucinogen-specific disorder, the specific contributory role of psychedelic drugs is unknown.
Cortical blindness is the total or partial loss of vision in a normal-appearing eye caused by damage to the brain's occipital cortex. Cortical blindness can be acquired or congenital, and may also be transient in certain instances. Acquired cortical blindness is most often caused by loss of blood flow to the occipital cortex from either unilateral or bilateral posterior cerebral artery blockage and by cardiac surgery. In most cases, the complete loss of vision is not permanent and the patient may recover some of their vision. Congenital cortical blindness is most often caused by perinatal ischemic stroke, encephalitis, and meningitis. Rarely, a patient with acquired cortical blindness may have little or no insight that they have lost vision, a phenomenon known as Anton–Babinski syndrome.
Akinetopsia, also known as cerebral akinetopsia or motion blindness, is a term introduced by Semir Zeki to describe an extremely rare neuropsychological disorder, having only been documented in a handful of medical cases, in which a patient cannot perceive motion in their visual field, despite being able to see stationary objects without issue. The syndrome is the result of damage to visual area V5, whose cells are specialized to detect directional visual motion. There are varying degrees of akinetopsia: from seeing motion as frames of a cinema reel to an inability to discriminate any motion. There is currently no effective treatment or cure for akinetopsia.
Focal neurologic signs also known as focal neurological deficits or focal CNS signs are impairments of nerve, spinal cord, or brain function that affects a specific region of the body, e.g. weakness in the left arm, the right leg, paresis, or plegia.

Posterior cortical atrophy (PCA), also called Benson's syndrome, is a rare form of dementia which is considered a visual variant or an atypical variant of Alzheimer's disease (AD). The disease causes atrophy of the posterior part of the cerebral cortex, resulting in the progressive disruption of complex visual processing. PCA was first described by D. Frank Benson in 1988.
Lesions in the visual pathway affect vision most often by creating deficits or negative phenomena, such as blindness, visual field deficits or scotomas, decreased visual acuity and color blindness. On occasion, they may also create false visual images, called positive visual phenomena. These images can be a result of distortion of incoming sensory information leading to an incorrect perception of a real image called an illusion. When the visual system produces images which are not based on sensory input, they can be referred to as hallucinations. The visual phenomena may last from brief moments to several hours, but they also can be permanent. They are generally associated with other symptoms but occasionally are isolated. Conditions causing these phenomena include disruptions in the visual input along the pathways lesions in the extracortical visual system, migraines, seizures, toxic-metabolic encephalopathy, psychiatric conditions and sleep apnea, among others. The mechanisms underlying positive visual phenomena are not yet well understood. Possible mechanisms may be: 1) defect in the sensory input causing compensatory upregulation of the visual cortex, 2) faulty visual processing in which inputs are normal but lesions result in an inappropriate pattern of cortical excitation, 3)variants of normal visual processing. Of all forms of hallucination, visual hallucinations are the least likely to be associated with psychiatric disorders. For example most patients with visual hallucinations do not have schizophrenia and most patients with schizophrenia do not have visual hallucinations.
Idiopathic childhood occipital epilepsy of Gastaut (ICOE-G) is a pure but rare form of idiopathic occipital epilepsy that affects otherwise normal children and adolescents. It is classified amongst benign idiopathic childhood focal epilepsies such as rolandic epilepsy and Panayiotopoulos syndrome.

Tactile hallucination is the false perception of tactile sensory input that creates a hallucinatory sensation of physical contact with an imaginary object. It is caused by the faulty integration of the tactile sensory neural signals generated in the spinal cord and the thalamus and sent to the primary somatosensory cortex (SI) and secondary somatosensory cortex (SII). Tactile hallucinations are recurrent symptoms of neurological diseases such as schizophrenia, Parkinson's disease, Ekbom's syndrome and delirium tremens. Patients who experience phantom limb pains also experience a type of tactile hallucination. Tactile hallucinations are also caused by drugs such as cocaine and alcohol.

Illusory palinopsia is a subtype of palinopsia, a visual disturbance defined as the persistence or recurrence of a visual image after the stimulus has been removed. Palinopsia is a broad term describing a heterogeneous group of symptoms, which is divided into hallucinatory palinopsia and illusory palinopsia. Illusory palinopsia is likely due to sustained awareness of a stimulus and is similar to a visual illusion: the distorted perception of a real external stimulus.
Hallucinatory palinopsia is a subtype of palinopsia, a visual disturbance defined as the persistent or recurrence of a visual image after the stimulus has been removed. Palinopsia is a broad term describing a group of symptoms which is divided into hallucinatory palinopsia and illusory palinopsia. Hallucinatory palinopsia refers to the projection of an already-encoded visual memory and is similar to a complex visual hallucination: the creation of a formed visual image where none exists.
Cerebral diplopia or polyopia describes seeing two or more images arranged in ordered rows, columns, or diagonals after fixation on a stimulus. The polyopic images occur monocular bilaterally and binocularly, differentiating it from ocular diplopia or polyopia. The number of duplicated images can range from one to hundreds. Some patients report difficulty in distinguishing the replicated images from the real images, while others report that the false images differ in size, intensity, or color. Cerebral polyopia is sometimes confused with palinopsia, in which multiple images appear while watching an object. However, in cerebral polyopia, the duplicated images are of a stationary object which are perceived even after the object is removed from the visual field. Movement of the original object causes all of the duplicated images to move, or the polyopic images disappear during motion. In palinoptic polyopia, movement causes each polyopic image to leave an image in its wake, creating hundreds of persistent images (entomopia).
Prosopometamorphopsia is a visual disorder characterized by altered perceptions of faces. In the perception of a person with the disorder, facial features are distorted in a variety of ways including drooping, swelling, discoloration, and shifts of position. Prosopometamorphopsia is distinct from prosopagnosia, which is characterised by the inability to recognise faces. About 75 cases of prosopometamorphopsia have been reported in the scientific literature. In about half of the reported cases, features on both sides of the face appear distorted. In the other half of cases, distortions are restricted to one side of the face and this condition is called hemi-prosopometamorphopsia.

Occipital epilepsy is a neurological disorder that arises from excessive neural activity in the occipital lobe of the brain that may or may not be symptomatic. Occipital lobe epilepsy is fairly rare, and may sometimes be misdiagnosed as migraine when symptomatic. Epileptic seizures are the result of synchronized neural activity that is excessive, and may stem from a failure of inhibitory neurons to regulate properly.
References
- 1 2 3 4 5 Bender, MB; Feldman, M; Sobin, AJ (Jun 1968). "Palinopsia". Brain: A Journal of Neurology. 91 (2): 321–38. doi:10.1093/brain/91.2.321. PMID 5721933.
- 1 2 Gersztenkorn, D; Lee, AG (Jul 2, 2014). "Palinopsia revamped: A systematic review of the literature". Survey of Ophthalmology. 60 (1): 1–35. doi:10.1016/j.survophthal.2014.06.003. PMID 25113609.
- 1 2 Arnold, RW; Janis, B; Wellman, S; Crouch, E; Rosen, C (Jan–Mar 1999). "Palinopsia with bacterial brain abscess and Noonan syndrome". Alaska Medicine. 41 (1): 3–7. PMID 10224677.
- ↑ Hayashi, R; Shimizu, S; Watanabe, R; Katsumata, Y; Mimura, M (Mar 2002). "Palinopsia and perilesional hyperperfusion following subcortical hemorrhage". Acta Neurologica Scandinavica. 105 (3): 228–31. doi: 10.1034/j.1600-0404.2002.1c217.x . PMID 11886369.
- ↑ Kupersmith, MJ; Berenstein, A; Nelson, PK; ApSimon, HT; Setton, A (Jan 1, 1999). "Visual symptoms with dural arteriovenous malformations draining into occipital veins". Neurology. 52 (1): 156–62. doi:10.1212/wnl.52.1.156. PMID 9921864. S2CID 28424667.
- ↑ Ogunyemi, A; Adams, D (May 1998). "Migraine-like symptoms triggered by occipital lobe seizures: response to sumatriptan". The Canadian Journal of Neurological Sciences. 25 (2): 151–3. doi: 10.1017/S0317167100033771 . PMID 9604138.
- ↑ Michel, EM; Troost, BT (Aug 1980). "Palinopsia: cerebral localization with computed tomography". Neurology. 30 (8): 887–9. doi:10.1212/wnl.30.8.887. PMID 7191073. S2CID 219197116.
- ↑ Engelsen, BA; Tzoulis, C; Karlsen, B; Lillebø, A; Laegreid, LM; Aasly, J; Zeviani, M; Bindoff, LA (Mar 2008). "POLG1 mutations cause a syndromic epilepsy with occipital lobe predilection". Brain: A Journal of Neurology. 131 (Pt 3): 818–28. doi: 10.1093/brain/awn007 . PMID 18238797.
- ↑ Purvin, V; Bonnin, J; Goodman, J (Dec 1989). "Palinopsia as a presenting manifestation of Creutzfeldt–Jakob disease". Journal of Clinical Neuro-ophthalmology. 9 (4): 242–6, discussion 247–8. PMID 2531161.
- ↑ Ossola, M; Romani, A; Tavazzi, E; Pichiecchio, A; Galimberti, CA (May 2010). "Epileptic mechanisms in Charles Bonnet syndrome". Epilepsy & Behavior. 18 (1–2): 119–22. doi:10.1016/j.yebeh.2010.03.010. PMID 20471325. S2CID 12737336.
- ↑ Hughes, MS; Lessell, S (Mar 1990). "Trazodone-induced palinopsia". Archives of Ophthalmology . 108 (3): 399–400. doi:10.1001/archopht.1990.01070050097040. PMID 2310343.
- ↑ Faber, RA; Benzick, JM (Apr 2000). "Nafazodone-induced palinopsia". Journal of Clinical Psychopharmacology. 20 (2): 275–6. doi:10.1097/00004714-200004000-00030. PMID 10770476.
- ↑ Ihde-Scholl, T; Jefferson, JW (May 2001). "Mitrazapine-associated palinopsia". The Journal of Clinical Psychiatry. 62 (5): 373. doi: 10.4088/jcp.v62n0512a . PMID 11411821.
- ↑ Fontenelle, LF (Spring 2008). "Topiramate-induced palinopsia". The Journal of Neuropsychiatry and Clinical Neurosciences. 20 (2): 249–50. doi:10.1176/jnp.2008.20.2.249. PMID 18451209.
- ↑ Purvin, VA (Apr 1995). "Visual disturbance secondary to clomiphene citrate". Archives of Ophthalmology. 113 (4): 482–4. doi:10.1001/archopht.1995.01100040102034. PMID 7710399.
- ↑ Lauterbach, EC; Abdelhamid, A; Annandale, JB (Jan 2000). "Posthallucinogen-like visual illusions (palinopsia) with risperidone in a patient without previous hallucinogen exposure: possible relation to serotonin 5HT2a receptor blockade". Pharmacopsychiatry. 33 (1): 38–41. doi:10.1055/s-2000-8452. PMID 10721882. S2CID 9009335.
- ↑ Stagno, SJ; Gates, TJ (1991). "Palinopsia: a review of the literature". Behavioural Neurology. 4 (2): 67–74. doi: 10.1155/1991/106585 . PMID 24487436.