An opportunistic infection is an infection caused by pathogens that take advantage of an opportunity not normally available. These opportunities can stem from a variety of sources, such as a weakened immune system, an altered microbiome, or breached integumentary barriers. Many of these pathogens do not necessarily cause disease in a healthy host that has a non-compromised immune system, and can, in some cases, act as commensals until the balance of the immune system is disrupted. Opportunistic infections can also be attributed to pathogens which cause mild illness in healthy individuals but lead to more serious illness when given the opportunity to take advantage of an immunocompromised host.
AIDS-defining clinical conditions is the list of diseases published by the Centers for Disease Control and Prevention (CDC) that are associated with AIDS and used worldwide as a guideline for AIDS diagnosis. CDC exclusively uses the term AIDS-defining clinical conditions, but the other terms remain in common use.

Atovaquone, sold under the brand name Mepron, is an antimicrobial medication for the prevention and treatment of Pneumocystis jirovecii pneumonia (PCP).

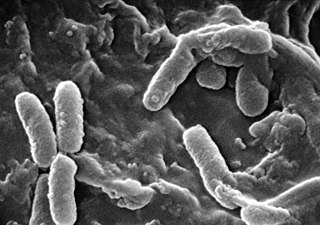
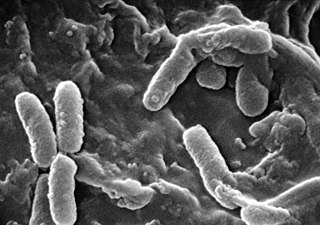
Stenotrophomonas maltophilia is an aerobic, nonfermentative, Gram-negative bacterium. It is an uncommon bacterium and human infection is difficult to treat. Initially classified as Bacterium bookeri, then renamed Pseudomonas maltophilia, S. maltophilia was also grouped in the genus Xanthomonas before eventually becoming the type species of the genus Stenotrophomonas in 1993.

A sputum culture is a test to detect and identify bacteria or fungi that infect the lungs or breathing passages. Sputum is a thick fluid produced in the lungs and in the adjacent airways. Normally, fresh morning sample is preferred for the bacteriological examination of sputum. A sample of sputum is collected in a sterile, wide-mouthed, dry, leak-proof and break-resistant plastic-container and sent to the laboratory for testing. Sampling may be performed by sputum being expectorated, induced, or taken via an endotracheal tube with a protected specimen brush in an intensive care setting. For selected organisms such as Cytomegalovirus or "Pneumocystis jiroveci" in specific clinical settings a bronchoalveolar lavage might be taken by an experienced pneumologist. If no bacteria or fungi grow, the culture is negative. If organisms that can cause the infection grow, the culture is positive. The type of bacterium or fungus is identified by microscopy, colony morphology and biochemical tests of bacterial growth.

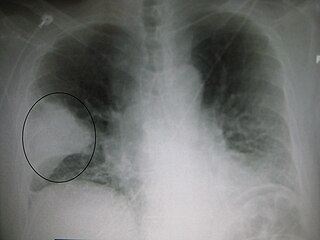
Pneumocystosis is a fungal infection that most often presents as Pneumocystis pneumonia in people with HIV/AIDS or poor immunity. It usually causes cough, difficulty breathing and fever, and can lead to respiratory failure. Involvement outside the lungs is rare but, can occur as a disseminated type affecting lymph nodes, spleen, liver, bone marrow, eyes, kidneys, thyroid, gastrointestinal tract or other organs. If occurring in the skin, it usually presents as nodular growths in the ear canals or underarms.
Pneumococcal pneumonia is a type of bacterial pneumonia that is caused by Streptococcus pneumoniae (pneumococcus). It is the most common bacterial pneumonia found in adults, the most common type of community-acquired pneumonia, and one of the common types of pneumococcal infection. The estimated number of Americans with pneumococcal pneumonia is 900,000 annually, with almost 400,000 cases hospitalized and fatalities accounting for 5-7% of these cases.
Otto Jírovec was a Czechoslovak professor of parasitology and protozoology.
Chlamydia felis is a Gram-negative, obligate intracellular bacterial pathogen that infects cats. It is endemic among domestic cats worldwide, primarily causing inflammation of feline conjunctiva, rhinitis and respiratory problems. C. felis can be recovered from the stomach and reproductive tract. Zoonotic infection of humans with C. felis has been reported. Strains FP Pring and FP Cello have an extrachromosomal plasmid, whereas the FP Baker strain does not. FP Cello produces lethal disease in mice, whereas the FP Baker does not. An attenuated FP Baker strain, and an attenuated 905 strain, are used as live vaccines for cats.

Hospital-acquired pneumonia (HAP) or nosocomial pneumonia refers to any pneumonia contracted by a patient in a hospital at least 48–72 hours after being admitted. It is thus distinguished from community-acquired pneumonia. It is usually caused by a bacterial infection, rather than a virus.

Pneumocystis jirovecii is a yeast-like fungus of the genus Pneumocystis. The causative organism of Pneumocystis pneumonia, it is an important human pathogen, particularly among immunocompromised hosts. Prior to its discovery as a human-specific pathogen, P. jirovecii was known as P. carinii.

Pneumocystis pneumonia (PCP), also known as Pneumocystis jirovecii pneumonia (PJP), is a form of pneumonia that is caused by the yeast-like fungus Pneumocystis jirovecii.

Enterobacter cloacae is a clinically significant Gram-negative, facultatively-anaerobic, rod-shaped bacterium.

Pathogenic bacteria are bacteria that can cause disease. This article focuses on the bacteria that are pathogenic to humans. Most species of bacteria are harmless and are often beneficial but others can cause infectious diseases. The number of these pathogenic species in humans is estimated to be fewer than a hundred. By contrast, several thousand species are part of the gut flora present in the digestive tract.
Pathogenic fungi are fungi that cause disease in humans or other organisms. Although fungi are eukaryotic, many pathogenic fungi are microorganisms. Approximately 300 fungi are known to be pathogenic to humans; their study is called "medical mycology". Fungal infections kill more people than either tuberculosis or malaria—about 2 million people per year.
Pseudomonas infection refers to a disease caused by one of the species of the genus Pseudomonas.
Antonio Carini (1872–1950) was an Italian physician, bacteriologist and professor. He worked in the public health services of São Paulo, Brazil for over forty years. Carini showed that rabies of herbivores could be transmitted by bats, and discovered a parasitic fungus, which causes pneumocystosis.
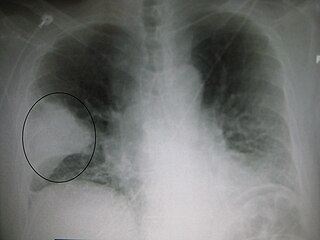
Pneumonia can be classified in several ways, most commonly by where it was acquired, but may also by the area of lung affected or by the causative organism. There is also a combined clinical classification, which combines factors such as age, risk factors for certain microorganisms, the presence of underlying lung disease or systemic disease and whether the person has recently been hospitalized.

T cell deficiency is a deficiency of T cells, caused by decreased function of individual T cells, it causes an immunodeficiency of cell-mediated immunity. T cells normal function is to help with the human body's immunity, they are one of the two primary types of lymphocytes(the other being B cells).
Pneumocystis wakefieldiae is a parasitic fungus isolated from rats.