Psilocybin is a naturally occurring psychedelic prodrug compound produced by more than 200 species of fungi. The most potent are members of genus Psilocybe, such as P. azurescens, P. semilanceata, and P. cyanescens, but psilocybin has also been isolated from about a dozen other genera. Psilocybin is itself biologically inactive but is quickly converted by the body to psilocin, which has mind-altering effects similar, in some aspects, to those of lysergic acid diethylamide (LSD), mescaline, and dimethyltryptamine (DMT). In general, the effects include euphoria, visual and mental hallucinations, changes in perception, distorted sense of time, and perceived spiritual experiences. It can also cause adverse reactions such as nausea and panic attacks.

Psychedelics are a subclass of hallucinogenic drugs whose primary effect is to trigger non-ordinary mental states and an apparent expansion of consciousness. Also referred to as classic hallucinogens or serotonergic hallucinogens, the term psychedelic is sometimes used more broadly to include various types of hallucinogens, such as those which are atypical or adjacent to psychedelia like salvia and MDMA, respectively.

Psilocybe cubensis, commonly known as the magic mushroom, shroom, golden halo, cube, or gold cap, is a species of psilocybin mushroom of moderate potency whose principal active compounds are psilocybin and psilocin. It belongs to the fungus family Hymenogastraceae and was previously known as Stropharia cubensis. It is the best-known psilocybin mushroom due to its wide distribution and ease of cultivation. This mushroom being optimal for home cultivation specifically, as was suggested in the 1970s, is primarily what led to P. cubensis being the psilocybin mushroom species most common on the black market as a street drug.

Psilocybin mushrooms, commonly known as magic mushrooms or shrooms, are a polyphyletic informal group of fungi that contain psilocybin, which turns into psilocin upon ingestion. Biological genera containing psilocybin mushrooms include Psilocybe, Panaeolus, Inocybe, Pluteus, Gymnopilus, and Pholiotina.

Psilocybe is a genus of gilled mushrooms, growing worldwide, in the family Hymenogastraceae. Many species contain the psychedelic compounds psilocybin and psilocin.
Psychedelic therapy refers to the proposed use of psychedelic drugs, such as psilocybin, MDMA, LSD, and ayahuasca, to treat mental disorders. As of 2021, psychedelic drugs are controlled substances in most countries and psychedelic therapy is not legally available outside clinical trials, with some exceptions.
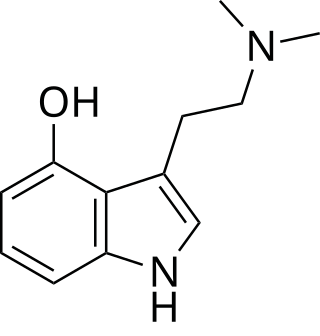
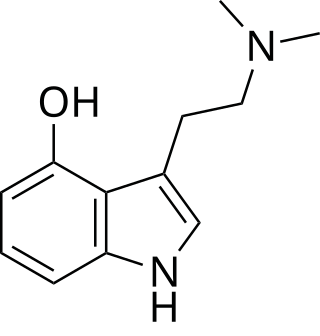
Psilocin is a substituted tryptamine alkaloid and a serotonergic psychedelic substance. It is present in most psychedelic mushrooms together with its phosphorylated counterpart psilocybin. Psilocin is a Schedule I drug under the Convention on Psychotropic Substances. Acting on the 5-HT2A receptors, psilocin modulates the production and reuptake of serotonin. The mind-altering effects of psilocin are highly variable and subjective and resemble those of LSD and DMT.
The Multidisciplinary Association for Psychedelic Studies (MAPS) is an American nonprofit organization working to raise awareness and understanding of psychedelic substances. MAPS was founded in 1986 by Rick Doblin and is now based in San Jose, California.
Treatment-resistant depression (TRD) is a term used in psychiatry to describe people with major depressive disorder (MDD) who do not respond adequately to a course of appropriate antidepressant medication within a certain time. Definitions of treatment-resistant depression vary, and they do not include a resistance to psychotherapy. Inadequate response has most commonly been defined as less than 50% reduction in depressive symptoms following treatment with at least one antidepressant medication, although definitions vary widely. Some other factors that may contribute to inadequate treatment are: a history of repeated or severe adverse childhood experiences, early discontinuation of treatment, insufficient dosage of medication, patient noncompliance, misdiagnosis, cognitive impairment, low income and other socio-economic variables, and concurrent medical conditions, including comorbid psychiatric disorders. Cases of treatment-resistant depression may also be referred to by which medications people with treatment-resistant depression are resistant to. In treatment-resistant depression adding further treatments such as psychotherapy, lithium, or aripiprazole is weakly supported as of 2019.

O-Acetylpsilocin is a semi-synthetic psychoactive drug that has been suggested by David Nichols to be a potentially useful alternative to psilocybin for pharmacological studies, as they are both believed to be prodrugs of psilocin. However, some users report that O-acetylpsilocin's subjective effects differ from those of psilocybin and psilocin. Additionally, some users prefer 4-AcO-DMT to natural psilocybin mushrooms due to feeling fewer adverse side effects such as nausea and heavy body load, which are more frequently reported in experiences involving natural mushrooms. It is the acetylated form of the psilocybin mushroom alkaloid psilocin and is a lower homolog of 4-AcO-MET, 4-AcO-DET, 4-AcO-MiPT and 4-AcO-DiPT.

Esketamine, sold under the brand names Spravato and Ketanest among others, is the S(+) enantiomer of ketamine. It is a dissociative hallucinogen drug used as a general anesthetic and as an antidepressant for treatment of depression. Esketamine is the active enantiomer of ketamine in terms of NMDA receptor antagonism and is more potent than racemic ketamine.

Drug policy of California refers to the policy on various classes and kinds of drugs in the U.S. state of California. Cannabis possession has been legalized with the Adult Use of Marijuana Act, passed in November 2016, with recreational sales starting January of the next year. With respect to many controlled substances, terms such as illegal and prohibited do not include their authorized possession or sale as laid out by applicable laws.
Management of depression is the treatment of depression that may involve a number of different therapies: medications, behavior therapy, psychotherapy, and medical devices.
The legal status of unauthorised actions with psilocybin mushrooms varies worldwide. Psilocybin and psilocin are listed as Schedule I drugs under the United Nations 1971 Convention on Psychotropic Substances. Schedule I drugs are defined as drugs with a high potential for abuse or drugs that have no recognized medical uses. However, psilocybin mushrooms have had numerous medicinal and religious uses in dozens of cultures throughout history and have a significantly lower potential for abuse than other Schedule I drugs.
Psychedelic microdosing involves consuming sub-threshold doses (microdoses) of serotonergic psychedelic drugs like LSD and psilocybin to potentially enhance creativity, energy, emotional balance, problem-solving abilities, and to address anxiety, depression, and addiction. This practice has gained popularity in the 21st century.

Magic truffles are the sclerotia of psilocybin mushrooms that are not technically the same as "mushrooms". They are masses of mycelium that contain the fruiting body which contains the hallucinogenic chemicals psilocybin and psilocin.
MDMA-assisted psychotherapy is the use of prescribed doses of MDMA as an adjunct to psychotherapy sessions. Research suggests that MDMA-assisted psychotherapy for post-traumatic stress disorder (PTSD), including Complex PTSD, might improve treatment effectiveness. In 2017, a Phase II clinical trial led to "breakthrough therapy" designation by the US Food and Drug Administration (FDA) for potential use as a treatment for PTSD.
Psychoplastogens are a group of small molecule drugs that produce rapid and sustained effects on neuronal structure and function, intended to manifest therapeutic benefit after a single administration. Several existing psychoplastogens have been identified and their therapeutic effects demonstrated; several are presently at various stages of development as medications including Ketamine, MDMA, Scopolamine, and the serotonergic psychedelics, including LSD, psilocin, DMT, and 5-MeO-DMT. Compounds of this sort are being explored as therapeutics for a variety of brain disorders including depression, addiction, and PTSD. The ability to rapidly promote neuronal changes via mechanisms of neuroplasticity was recently discovered as the common therapeutic activity and mechanism of action.
Psychedelic treatments for trauma-related disorders are the use of psychedelic substances, either alone or used in conjunction with psychotherapy, to treat trauma-related disorders. Trauma-related disorders, such as post-traumatic stress disorder (PTSD), have a lifetime prevalence of around 8% in the US population. However, even though trauma-related disorders can hinder the everyday life of individuals with them, less than 50% of patients who meet criteria for PTSD diagnosis receive proper treatment. Psychotherapy is an effective treatment for trauma-related disorders. A meta-analysis of treatment outcomes has shown that 67% of patients who completed treatment for PTSD no longer met diagnostic criteria for PTSD. For those seeking evidence-based psychotherapy treatment, it is estimated that 22-24% will drop out of their treatment. In addition to psychotherapy, pharmacotherapy (medication) is an option for treating PTSD; however, research has found that pharmacotherapy is only effective for about 59% of patients. Although both forms of treatment are effective for many patients, high dropout rates of psychotherapy and treatment-resistant forms of PTSD have led to increased research in other possible forms of treatment. One such form is the use of psychedelics.
California Sober is a recovery model that incorporates the use of psychedelic therapy, along with meditation and exercise, with the intent of abstaining from more harmful and addictive substances. The difference between the California Sober and traditional recovery systems, such as Narcotics Anonymous, is that it doesn't require Asceticism, allowing the practitioner to use substances with little to no potential for addiction in such a way that those substances are said to aid in the recovery process.