Health care reform is for the most part governmental policy that affects health care delivery in a given place. Health care reform typically attempts to:

Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. The term includes work done in providing primary care, secondary care, and tertiary care, as well as in public health.

Primary care is the day-to-day healthcare given by a health care provider. Typically this provider acts as the first contact and principal point of continuing care for patients within a healthcare system, and coordinates other specialist care that the patient may need. Patients commonly receive primary care from professionals such as a primary care physician, a physician assistant, a physical therapist, or a nurse practitioner. In some localities, such a professional may be a registered nurse, a pharmacist, a clinical officer, or an Ayurvedic or other traditional medicine professional. Depending on the nature of the health condition, patients may then be referred for secondary or tertiary care.
Universal health care is a health care system in which all residents of a particular country or region are assured access to health care. It is generally organized around providing either all residents or only those who cannot afford on their own, with either health services or the means to acquire them, with the end goal of improving health outcomes.

A clinic is a health facility that is primarily focused on the care of outpatients. Clinics can be privately operated or publicly managed and funded. They typically cover the primary care needs of populations in local communities, in contrast to larger hospitals which offer more specialized treatments and admit inpatients for overnight stays.
Health care in Ireland is delivered through public and private healthcare. The public health care system is governed by the Health Act 2004, which established a new body to be responsible for providing health and personal social services to everyone living in Ireland – the Health Service Executive. The new national health service came into being officially on 1 January 2005; however the new structures are currently in the process of being established as the reform programme continues. In addition to the public-sector, there is also a large private healthcare market.
The Cuban government operates a national health system and assumes fiscal and administrative responsibility for the health care of all its citizens. All healthcare in Cuba is free to Cuban residents, although challenges include low salaries for doctors, poor facilities, poor provision of equipment, and the frequent absence of essential drugs. There are no private hospitals or clinics as all health services are government-run. The current public health minister of Cuba is José Angel Portal Miranda.
A public hospital, or government hospital, is a hospital which is government owned and is fully funded by the government and operates solely off the money that is collected from taxpayers to fund healthcare initiatives. In almost all the developed countries but the United States of America, and in most of the developing countries, this type of hospital provides medical care free of charge to patients, covering expenses and wages by government reimbursement.

Health care in Saudi Arabia is a national health care system in which the government provides free universal healthcare coverage through a number of government agencies. There is also a growing role and increased participation from the private sector in the provision of health care services. Saudi Arabia has been ranked among the 26 best countries in providing high quality healthcare.
The healthcare reform in China refers to the previous and ongoing healthcare system transition in modern China. China's government, specifically the National Health and Family Planning Commission, plays a leading role in these reforms. Reforms focus on establishing public medical insurance systems and enhancing public healthcare providers, the main component in China's healthcare system. In urban and rural areas, three government medical insurance systems—Urban Residents Basic Medical Insurance, Urban Employee Basic Medical Insurance, and the New Rural Co-operative Medical Scheme—cover almost everyone. Various public healthcare facilities, including county or city hospitals, community health centers, and township health centers, were founded to serve diverse needs. Current and future reforms are outlined in Healthy China 2030.
Healthcare in Brazil is a constitutional right. It is provided by both private and government institutions. The Health Minister administers national health policy. Primary healthcare remains the responsibility of the federal government, elements of which are overseen by individual states. Public healthcare is provided to all Brazilian permanent residents and foreigners in Brazilian territory through the National Healthcare System, known as the Unified Health System. The SUS is universal and free for everyone.
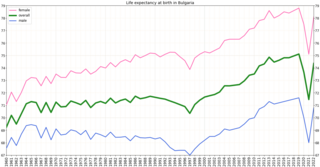
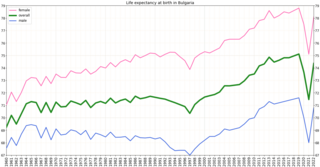
Bulgaria had the third highest mortality in Europe, at 708 per 100,000 population in 2015. The four European regions with the highest death rates from diseases of the circulatory system were all in Bulgaria. In the early 2000s, the major natural causes of death were cardiovascular disease, cancer, and respiratory illness. Bulgaria has had a very low incidence rate of human immunodeficiency virus (HIV). Although in 2003 the estimated rate of incidence was less than 0.1 percent of the population, in the early 2000s the number of new case reports increased annually. In 2005 some 86 new cases were reported, bringing the official total to about 600, and 58 new cases were reported in the first half of 2006. In 2010, there were 1,160 HIV-positive persons.

Healthcare in Russia is provided by the state through the Federal Compulsory Medical Insurance Fund, and regulated through the Ministry of Health. The Constitution of the Russian Federation has provided all citizens the right to free healthcare since 1993. In 2008, 621,000 doctors and 1.3 million nurses were employed in Russian healthcare. The number of doctors per 10,000 people was 43.8, but only 12.1 in rural areas. The number of general practitioners as a share of the total number of doctors was 1.26 percent. There are about 9.3 beds per thousand population—nearly double the OECD average.
Healthcare in Finland consists of a highly decentralized three-level publicly funded healthcare system and a much smaller private sector. Although the Ministry of Social Affairs and Health has the highest decision-making authority, specific healthcare precincts are responsible for providing healthcare to their residents as of 2023.
The French health care system is one of universal health care largely financed by government national health insurance. In its 2000 assessment of world health care systems, the World Health Organization found that France provided the "best overall health care" in the world. In 2017, France spent 11.3% of GDP on health care, or US$5,370 per capita, a figure higher than the average spent by rich countries, though similar to Germany (10.6%) and Canada (10%), but much less than in the US. Approximately 77% of health expenditures are covered by government funded agencies.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).

Healthcare in Denmark is largely provided by the local governments of the five regions, with coordination and regulation by central government, while nursing homes, home care, and school health services are the responsibility of the 98 municipalities. Some specialised hospital services are managed centrally.
Examples of health care systems of the world, sorted by continent, are as follows.

As of 2019 Lithuanian life expectancy at birth was 76.0 and the infant mortality rate was 2.99 per 1,000 births. This is below the EU and OECD average.

Healthcare in Azerbaijan is provided by public and private healthcare institutions and regulated through the Ministry of Healthcare.