The brachial plexus is a network of nerves formed by the anterior rami of the lower four cervical nerves and first thoracic nerve. This plexus extends from the spinal cord, through the cervicoaxillary canal in the neck, over the first rib, and into the armpit, it supplies afferent and efferent nerve fibers to the chest, shoulder, arm, forearm, and hand.

A breech birth is when a baby is born bottom first instead of head first, as is normal. Around 3–5% of pregnant women at term have a breech baby. Due to their higher than average rate of possible complications for the baby, breech births are generally considered higher risk. Breech births also occur in many other mammals such as dogs and horses, see veterinary obstetrics.

Umbilical cord prolapse is when the umbilical cord comes out of the uterus with or before the presenting part of the baby. The concern with cord prolapse is that pressure on the cord from the baby will compromise blood flow to the baby. It usually occurs during labor but can occur anytime after the rupture of membranes.

Large for gestational age (LGA) is a term used to describe infants that are born with an abnormally high weight, specifically in the 90th percentile or above, compared to other babies of the same developmental age. Macrosomia is a similar term that describes excessive birth weight, but refers to an absolute measurement, regardless of gestational age. Typically the threshold for diagnosing macrosomia is a body weight between 4,000 and 4,500 grams, or more, measured at birth, but there are difficulties reaching a universal agreement of this definition.
Obstructed labour, also known as labour dystocia, is the baby not exiting the pelvis because it is physically blocked during childbirth although the uterus contracts normally. Complications for the baby include not getting enough oxygen which may result in death. It increases the risk of the mother getting an infection, having uterine rupture, or having post-partum bleeding. Long-term complications for the mother include obstetrical fistula. Obstructed labour is said to result in prolonged labour, when the active phase of labour is longer than 12 hours.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.
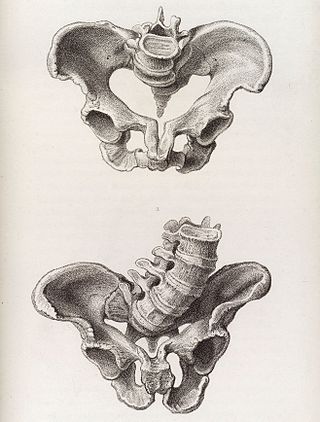
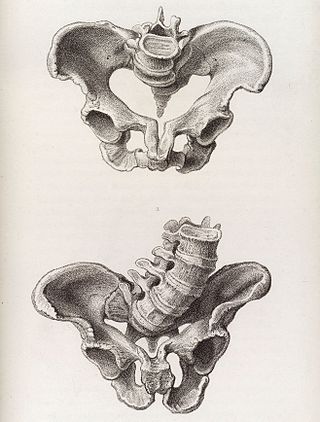
The obstetrical dilemma is a hypothesis to explain why humans often require assistance from other humans during childbirth to avoid complications, whereas most non-human primates give birth unassisted with relatively little difficulty. This occurs due to the tight fit of the fetal head to the maternal birth canal, which is additionally convoluted, meaning the head and therefore body of the infant must rotate during childbirth in order to fit, unlike in other, non-upright walking mammals. Consequently, there is an unusually high incidence of cephalopelvic disproportion and obstructed labor in humans.
Postterm pregnancy is when a woman has not yet delivered her baby after 42 weeks of gestation, two weeks beyond the typical 40-week duration of pregnancy. Postmature births carry risks for both the mother and the baby, including fetal malnutrition, meconium aspiration syndrome, and stillbirths. After the 42nd week of gestation, the placenta, which supplies the baby with nutrients and oxygen from the mother, starts aging and will eventually fail. Postterm pregnancy is a reason to induce labor.
The Zavanelli maneuver is an obstetric maneuver that involves pushing back the delivered fetal head into the birth canal in anticipation of performing a cesarean section in cases of shoulder dystocia.

Obstetrical forceps are a medical instrument used in childbirth. Their use can serve as an alternative to the ventouse method.
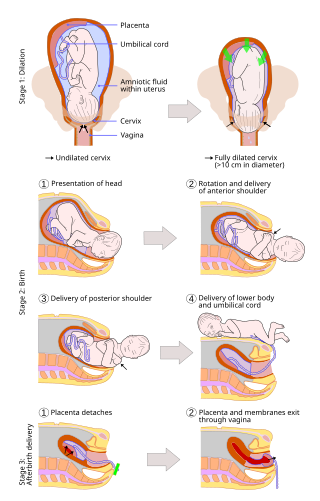
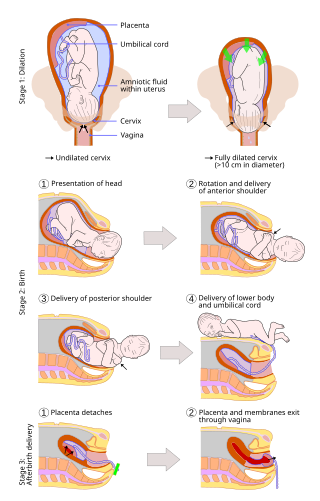
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, with lower morbidity and mortality than caesarean sections (C-sections).
An asynclitic birth or asynclitism are terms used in obstetrics to refer to childbirth in which there is malposition of the head of the fetus in the uterus, relative to the birth canal. Asynclitic presentation is different from a shoulder presentation, in which the shoulder is presenting first. Many babies enter the pelvis in an asynclitic presentation, and most asynclitism corrects spontaneously as part of the normal birthing process.

The McRoberts maneuver is an obstetrical maneuver used to assist in childbirth. It is named after William A. McRoberts, Jr. It is employed in case of shoulder dystocia during childbirth and involves hyperflexing the mother's legs tightly to her abdomen. It is effective due to the increased mobility at the sacroiliac joint during pregnancy, allowing rotation of the pelvis and facilitating the release of the fetal shoulder. If this maneuver does not succeed, an assistant applies pressure on the lower abdomen. Current guidelines strongly recommend against pulling on the infants head, as this could lead to brachial plexus injury. Instead, support while keeping the neck straight is indicated. The technique is effective in about 42% of cases. Note that suprapubic pressure and McRobert's maneuver together will resolve 90% of cases.
Wood's screw maneuver is practiced in obstetrics when dealing with shoulder dystocia – a condition in which the fetal shoulders cannot easily pass through the vagina. In this maneuver the anterior shoulder is pushed towards the baby's chest, and the posterior shoulder is pushed towards the baby's back, making the baby's head somewhat face the mother's rectum.

In obstetrics, the presentation of a fetus about to be born specifies which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal. According to the leading part, this is identified as a cephalic, breech, or shoulder presentation. A malpresentation is any presentation other than a vertex presentation.

A shoulder presentation is a malpresentation at childbirth where the baby is in a transverse lie, thus the leading part is an arm, a shoulder, or the trunk. While a baby can be delivered vaginally when either the head or the feet/buttocks are the leading part, it usually cannot be expected to be delivered successfully with a shoulder presentation unless a cesarean section (C/S) is performed.
An obstetric labor complication is a difficulty or abnormality that arises during the process of labor or delivery.

Rubin's I and II maneuvers, rotational maneuver to deliver the baby in case of shoulder dystocia.

Emergency childbirth is the precipitous birth of an infant in an unexpected setting. In planned childbirth, mothers choose the location and obstetric team ahead of time. Options range from delivering at home, at a hospital, a medical facility or a birthing center. Sometimes, birth can occur on the way to these facilities, without a healthcare team. The rates of unplanned childbirth are low. If the birth is imminent, emergency measures may be needed. Emergency services can be contacted for help in some countries.

Operative vaginal delivery, also known as assisted or instrumental vaginal delivery, is a vaginal delivery that is assisted by the use of forceps or a vacuum extractor.