Sleep is a state of reduced mental and physical activity in which consciousness is altered and sensory activity is inhibited to a certain extent. During sleep, there is a decrease in muscle activity, and interactions with the surrounding environment. While sleep differs from wakefulness in terms of the ability to react to stimuli, it still involves active brain patterns, making it more reactive than a coma or disorders of consciousness.

A sleep disorder, or somnipathy, is a medical disorder of an individual's sleep patterns. Some sleep disorders are severe enough to interfere with normal physical, mental, social and emotional functioning. Sleep disorders are frequent and can have serious consequences on patients’ health and quality of life. Polysomnography and actigraphy are tests commonly ordered for diagnosing sleep disorders.
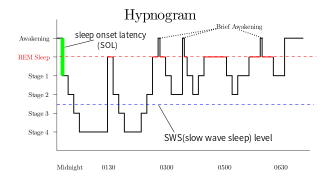
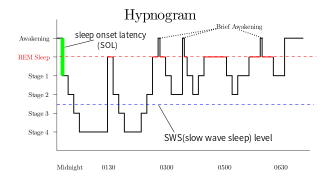
Rapid eye movement sleep is a unique phase of sleep in mammals and birds, characterized by random rapid movement of the eyes, accompanied by low muscle tone throughout the body, and the propensity of the sleeper to dream vividly.
In psychology, a mood is an affective state. In contrast to emotions or feelings, moods are less specific, less intense and less likely to be provoked or instantiated by a particular stimulus or event. Moods are typically described as having either a positive or negative valence. In other words, people usually talk about being in a good mood or a bad mood. There are many different factors that influence mood, and these can lead to positive or negative effects on mood.

A mood swing is an extreme or sudden change of mood. Such changes can play a positive part in promoting problem solving and in producing flexible forward planning, or be disruptive. When mood swings are severe, they may be categorized as part of a mental illness, such as bipolar disorder, where erratic and disruptive mood swings are a defining feature.
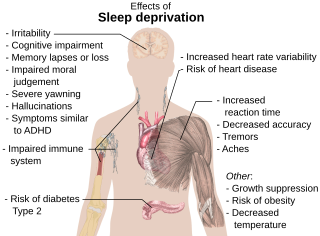
Sleep debt or sleep deficit is the cumulative effect of not getting enough sleep. A large sleep debt may lead to mental or physical fatigue, and can adversely affect one's mood, energy, and ability to think clearly.
Wake therapy is a specific application of intentional sleep deprivation. It encompasses many sleep-restricting paradigms that aim to address mood disorders with a form of non-pharmacological therapy.
Irritability is the excitatory ability that living organisms have to respond to changes in their environment. The term is used for both the physiological reaction to stimuli and for the pathological, abnormal or excessive sensitivity to stimuli.
Reduced affect display, sometimes referred to as emotional blunting or emotional numbing, is a condition of reduced emotional reactivity in an individual. It manifests as a failure to express feelings either verbally or nonverbally, especially when talking about issues that would normally be expected to engage emotions. In this condition, expressive gestures are rare and there is little animation in facial expression or vocal inflection. Additionally, reduced affect can be symptomatic of autism, schizophrenia, depression, post-traumatic stress disorder, depersonalization disorder, schizoid personality disorder or brain damage. It may also be a side effect of certain medications.
Emotional dysregulation is a range of emotional responses that do not lie within a desirable scope of emotive response, considering the stimuli.
In the study of psychology, neuroticism has been considered a fundamental personality trait. In the Big Five approach to personality trait theory, individuals with high scores for neuroticism are more likely than average to be moody and to experience such feelings as anxiety, worry, fear, anger, frustration, envy, jealousy, pessimism, guilt, depressed mood, and loneliness. Such people are thought to respond worse to stressors and are more likely to interpret ordinary situations, such as minor frustrations, as appearing hopelessly difficult. The responses can include maladaptive behaviors, such as dissociation, procrastination, substance use, etc., which aids in relieving the negative emotions and generating positive ones.
Emotional self-regulation or emotion regulation is the ability to respond to the ongoing demands of experience with the range of emotions in a manner that is socially tolerable and sufficiently flexible to permit spontaneous reactions as well as the ability to delay spontaneous reactions as needed. It can also be defined as extrinsic and intrinsic processes responsible for monitoring, evaluating, and modifying emotional reactions. Emotional self-regulation belongs to the broader set of emotion regulation processes, which includes both the regulation of one's own feelings and the regulation of other people's feelings.

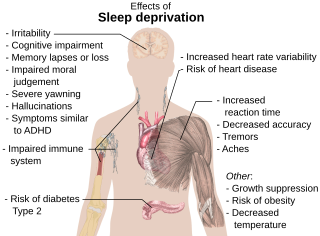
Sleep deprivation, also known as sleep insufficiency or sleeplessness, is the condition of not having adequate duration and/or quality of sleep to support decent alertness, performance, and health. It can be either chronic or acute and may vary widely in severity. All known animals sleep or exhibit some form of sleep behavior, and the importance of sleep is self-evident for humans, as nearly a third of a person's life is spent sleeping.
Emotional responsivity is the ability to acknowledge an affective stimuli by exhibiting emotion. It is a sharp change of emotion according to a person's emotional state. Increased emotional responsivity refers to demonstrating more response to a stimulus. Reduced emotional responsivity refers to demonstrating less response to a stimulus. Any response exhibited after exposure to the stimulus, whether it is appropriate or not, would be considered as an emotional response. Although emotional responsivity applies to nonclinical populations, it is more typically associated with individuals with schizophrenia and autism.
Scientific studies have found that different brain areas show altered activity in humans with major depressive disorder (MDD), and this has encouraged advocates of various theories that seek to identify a biochemical origin of the disease, as opposed to theories that emphasize psychological or situational causes. Factors spanning these causative groups include nutritional deficiencies in magnesium, vitamin D, and tryptophan with situational origin but biological impact. Several theories concerning the biologically based cause of depression have been suggested over the years, including theories revolving around monoamine neurotransmitters, neuroplasticity, neurogenesis, inflammation and the circadian rhythm. Physical illnesses, including hypothyroidism and mitochondrial disease, can also trigger depressive symptoms.

The neuroscience of sleep is the study of the neuroscientific and physiological basis of the nature of sleep and its functions. Traditionally, sleep has been studied as part of psychology and medicine. The study of sleep from a neuroscience perspective grew to prominence with advances in technology and the proliferation of neuroscience research from the second half of the twentieth century.
Sleep disorder is a common repercussion of traumatic brain injury (TBI). It occurs in 30%-70% of patients with TBI. TBI can be distinguished into two categories, primary and secondary damage. Primary damage includes injuries of white matter, focal contusion, cerebral edema and hematomas, mostly occurring at the moment of the trauma. Secondary damage involves the damage of neurotransmitter release, inflammatory responses, mitochondrial dysfunctions and gene activation, occurring minutes to days following the trauma. Patients with sleeping disorders following TBI specifically develop insomnia, sleep apnea, narcolepsy, periodic limb movement disorder and hypersomnia. Furthermore, circadian sleep-wake disorders can occur after TBI.

Sleep is a naturally recurring state of mind and body, characterized by altered consciousness, relatively inhibited sensory activity, reduced muscle activity, and inhibition of nearly all voluntary muscles during rapid eye movement (REM) sleep, and reduced interactions with surroundings. An essential aspect of sleep is that it provides the human body with a period of reduced functioning that allows for the systems throughout the body to be repaired. This time allows for the body to recharge and return to a phase of optimal functioning. It is recommended that adults get 7 to 9 hours of sleep each night. Sleep is regulated by an internal process known as the circadian rhythm. This 24-hour cycle regulates periods of alertness and tiredness that an individual experiences. The correlation between psychological stress and sleep is complex and not fully understood. In fact, many studies have found a bidirectional relationship between stress and sleep. This means that sleep quality can affect stress levels, and stress levels can affect sleep quality. Sleep change depends on the type of stressor, sleep perception, related psychiatric conditions, environmental factors, and physiological limits.
Sleep is known to play an important role in the etiology and maintenance of bipolar disorder. Patients with bipolar disorder often have a less stable and more variable circadian activity. Circadian activity disruption can be apparent even if the person concerned is not currently ill.
Affect labeling is an implicit emotional regulation strategy that can be simply described as "putting feelings into words". Specifically, it refers to the idea that explicitly labeling one's, typically negative, emotional state results in a reduction of the conscious experience, physiological response, and/or behavior resulting from that emotional state. For example, writing about a negative experience in one's journal may improve one's mood. Some other examples of affect labeling include discussing one's feelings with a therapist, complaining to friends about a negative experience, posting one's feelings on social media or acknowledging the scary aspects of a situation.