Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.

The respiratory system is a biological system consisting of specific organs and structures used for gas exchange in animals and plants. The anatomy and physiology that make this happen varies greatly, depending on the size of the organism, the environment in which it lives and its evolutionary history. In land animals, the respiratory surface is internalized as linings of the lungs. Gas exchange in the lungs occurs in millions of small air sacs; in mammals and reptiles, these are called alveoli, and in birds, they are known as atria. These microscopic air sacs have a very rich blood supply, thus bringing the air into close contact with the blood. These air sacs communicate with the external environment via a system of airways, or hollow tubes, of which the largest is the trachea, which branches in the middle of the chest into the two main bronchi. These enter the lungs where they branch into progressively narrower secondary and tertiary bronchi that branch into numerous smaller tubes, the bronchioles. In birds, the bronchioles are termed parabronchi. It is the bronchioles, or parabronchi that generally open into the microscopic alveoli in mammals and atria in birds. Air has to be pumped from the environment into the alveoli or atria by the process of breathing which involves the muscles of respiration.

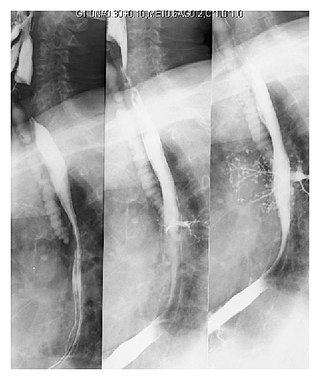
The trachea, also known as the windpipe, is a cartilaginous tube that connects the larynx to the bronchi of the lungs, allowing the passage of air, and so is present in almost all animals with lungs. The trachea extends from the larynx and branches into the two primary bronchi. At the top of the trachea the cricoid cartilage attaches it to the larynx. The trachea is formed by a number of horseshoe-shaped rings, joined together vertically by overlying ligaments, and by the trachealis muscle at their ends. The epiglottis closes the opening to the larynx during swallowing.
Diffusing capacity of the lung (DL) measures the transfer of gas from air in the lung, to the red blood cells in lung blood vessels. It is part of a comprehensive series of pulmonary function tests to determine the overall ability of the lung to transport gas into and out of the blood. DL, especially DLCO, is reduced in certain diseases of the lung and heart. DLCO measurement has been standardized according to a position paper by a task force of the European Respiratory and American Thoracic Societies.

The respiratory tract is the subdivision of the respiratory system involved with the process of respiration in mammals. The respiratory tract is lined with respiratory epithelium as respiratory mucosa.
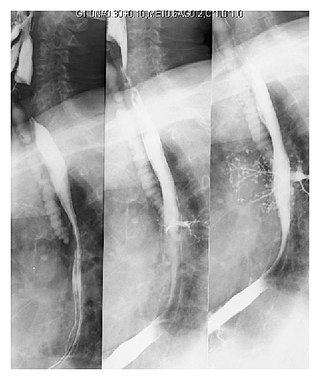
Pulmonary aspiration is the entry of material such as pharyngeal secretions, food or drink, or stomach contents from the oropharynx or gastrointestinal tract, into the larynx and lower respiratory tract, the portions of the respiratory system from the trachea (windpipe) to the lungs. A person may inhale the material, or it may be delivered into the tracheobronchial tree during positive pressure ventilation. When pulmonary aspiration occurs during eating and drinking, the aspirated material is often colloquially referred to as "going down the wrong pipe".

Inhalation is the process of drawing air or other gases into the respiratory tract, primarily for the purpose of breathing and oxygen exchange within the body. It is a fundamental physiological function in humans and many other organisms, essential for sustaining life. Inhalation is the first phase of respiration, allowing the exchange of oxygen and carbon dioxide between the body and the environment, vital for the body's metabolic processes. This article delves into the mechanics of inhalation, its significance in various contexts, and its potential impact on health.

Carbon monoxide poisoning typically occurs from breathing in carbon monoxide (CO) at excessive levels. Symptoms are often described as "flu-like" and commonly include headache, dizziness, weakness, vomiting, chest pain, and confusion. Large exposures can result in loss of consciousness, arrhythmias, seizures, or death. The classically described "cherry red skin" rarely occurs. Long-term complications may include chronic fatigue, trouble with memory, and movement problems.
In physiology, respiration is the movement of oxygen from the outside environment to the cells within tissues, and the removal of carbon dioxide in the opposite direction to the surrounding environment.

Oxygen therapy, also referred to as supplemental oxygen, is the use of oxygen as medical treatment. Supplemental oxygen can also refer to the use of oxygen enriched air at altitude. Acute indications for therapy include hypoxemia, carbon monoxide toxicity and cluster headache. It may also be prophylactically given to maintain blood oxygen levels during the induction of anesthesia. Oxygen therapy is often useful in chronic hypoxemia caused by conditions such as severe COPD or cystic fibrosis. Oxygen can be delivered via nasal cannula, face mask, or endotracheal intubation at normal atmospheric pressure, or in a hyperbaric chamber. It can also be given through bypassing the airway, such as in ECMO therapy.

An injury is any physiological damage to living tissue caused by immediate physical stress. Injuries to humans can occur intentionally or unintentionally and may be caused by blunt trauma, penetrating trauma, burning, toxic exposure, asphyxiation, or overexertion. Injuries can occur in any part of the body, and different symptoms are associated with different injuries.

Respiratory arrest is a serious medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.
A blood agent is a toxic chemical agent that affects the body by being absorbed into the blood. Blood agents are fast-acting, potentially lethal poisons that typically manifest at room temperature as volatile colorless gases with a faint odor. They are either cyanide- or arsenic-based.
Diving disorders, or diving related medical conditions, are conditions associated with underwater diving, and include both conditions unique to underwater diving, and those that also occur during other activities. This second group further divides into conditions caused by exposure to ambient pressures significantly different from surface atmospheric pressure, and a range of conditions caused by general environment and equipment associated with diving activities.
Occupational lung diseases comprise a broad group of diseases, including occupational asthma, industrial bronchitis, chronic obstructive pulmonary disease (COPD), bronchiolitis obliterans, inhalation injury, interstitial lung diseases, infections, lung cancer and mesothelioma. These can be caused directly or due to immunological response to an exposure to a variety of dusts, chemicals, proteins or organisms. Occupational cases of interstitial lung disease may be misdiagnosed as COPD, idiopathic pulmonary fibrosis, or a myriad of other diseases; leading to a delay in identification of the causative agent.
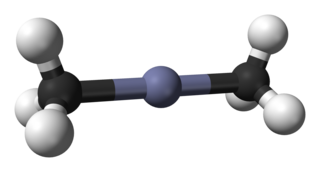
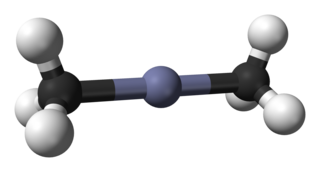
Dimethylzinc, also known as zinc methyl, DMZ, or DMZn, is an organozinc compound with the chemical formula Zn(CH3)2. It belongs to the large series of similar compounds such as diethylzinc.

Tracheobronchial injury is damage to the tracheobronchial tree. It can result from blunt or penetrating trauma to the neck or chest, inhalation of harmful fumes or smoke, or aspiration of liquids or objects.
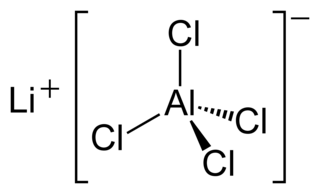
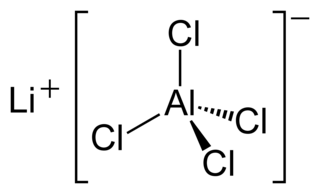
Lithium tetrachloroaluminate is an inorganic compound with the formula Li[AlCl4]. It consists of lithium cations Li+ and tetrahedral tetrachloroaluminate anions [AlCl4]−.
Acute inhalation injury may result from frequent and widespread use of household cleaning agents and industrial gases. The airways and lungs receive continuous first-pass exposure to non-toxic and irritant or toxic gases via inhalation. Irritant gases are those that, on inhalation, dissolve in the water of the respiratory tract mucosa and provoke an inflammatory response, usually from the release of acidic or alkaline radicals. Smoke, chlorine, phosgene, sulfur dioxide, hydrogen chloride, hydrogen sulfide, nitrogen dioxide, ozone, and ammonia are common irritants.

A hydrofluoric acid burn is a chemical burn from hydrofluoric acid. Where it contacts the skin it results in significant pain, swelling, redness, and skin breakdown. If the fumes are breathed in swelling of the upper airway and bleeding may occur. Complications can include electrolyte, heart, lung, kidney, and neurological problems.