A transient ischemic attack (TIA), commonly known as a mini-stroke, is a minor stroke whose noticeable symptoms usually end in less than an hour. TIA causes the same symptoms associated with strokes, such as weakness or numbness on one side of the body, sudden dimming or loss of vision, difficulty speaking or understanding language, slurred speech, or confusion.

An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance. The emergency department is usually found in a hospital or other primary care center.

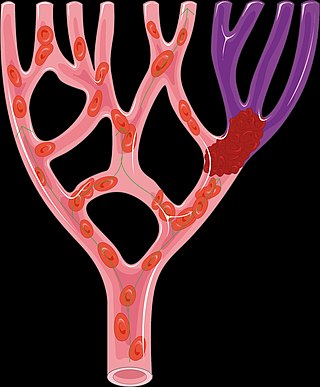
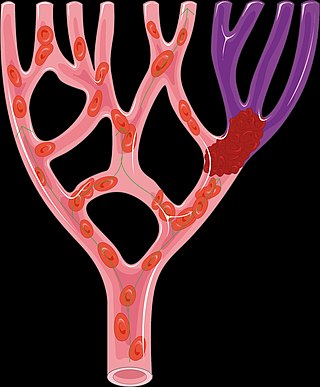
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.
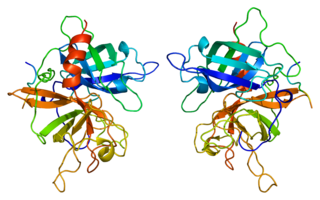
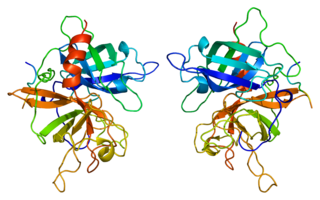
Tissue-type plasminogen activator, short name tPA, is a protein that facilitates the breakdown of blood clots. It acts as an enzyme to convert plasminogen into its active form plasmin, the major enzyme responsible for clot breakdown. It is a serine protease found on endothelial cells lining the blood vessels. Human tPA is encoded by the PLAT gene, and has a molecular weight of ~70 kDa in the single-chain form.
Mechanical thrombectomy, or simply thrombectomy, is the removal of a blood clot (thrombus) from a blood vessel, often and especially endovascularly as an interventional radiology procedure called endovascular thrombectomy (EVT). It thus contrasts with thrombolysis by thrombolytic medications, as either alternative or complement thereto. It is commonly performed in the cerebral arteries as treatment to reverse the ischemia in some ischemic strokes. Open vascular surgery versions of thrombectomy also exist. The effectiveness of thrombectomy for strokes was confirmed in several randomised clinical trials conducted at various medical centers throughout the United States, as reported in a seminal multistudy report in 2015.
Alteplase, sold under the brand name Activase among others, is a biosynthetic form of human tissue-type plasminogen activator (t-PA). It is a thrombolytic medication used to treat acute ischemic stroke, acute ST-elevation myocardial infarction, pulmonary embolism associated with low blood pressure, and blocked central venous catheter. It is given by injection into a vein or artery. Alteplase is the same as the normal human plasminogen activator produced in vascular endothelial cells and is synthesized via recombinant DNA technology in Chinese hamster ovary cells (CHO). Alteplase causes the breakdown of a clot by inducing fibrinolysis.

Carotid artery stenosis is a narrowing or constriction of any part of the carotid arteries, usually caused by atherosclerosis.

Desmoteplase is a novel, highly fibrin-specific "clot-busting" (thrombolytic) drug in development that reached phase III clinical trials. The Danish pharmaceutical company, Lundbeck, owns the worldwide rights to Desmoteplase. In 2009, two large trials were started to test it as a safe and effective treatment for patients with acute ischaemic stroke. After disappointing results in DIAS-3, DIAS-4 was terminated, and in December 2014 Lundbeck announced that they would stop the development of desmoteplase.

Cerebral infarction is the pathologic process that results in an area of necrotic tissue in the brain. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia), most commonly due to thromboembolism, and manifests clinically as ischemic stroke. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.

The Queen's Medical Center, originally named and still commonly referred to as Queen's Hospital, is the largest private non-profit hospital in Honolulu, Hawaii. The institution was founded in 1859 by Queen Emma and King Kamehameha IV, and is located in Downtown Honolulu.

Emergency nursing is a specialty within the field of professional nursing focusing on the care of patients who require prompt medical attention to avoid long-term disability or death. In addition to addressing "true emergencies," emergency nurses increasingly care for people who are unwilling or unable to get primary medical care elsewhere and come to emergency departments for help. In fact, only a small percentage of emergency department (ED) patients have emergency conditions such as a stroke, heart attack or major trauma. Emergency nurses also tend to patients with acute alcohol and/or drug intoxication, psychiatric and behavioral problems and those who have been raped.

CHA Hollywood Presbyterian Medical Center, formerly known as Queen of Angels – Hollywood Presbyterian Medical Center, is a private hospital located at 1300 North Vermont Avenue in Los Angeles, California. The hospital has 434 beds and is owned by the South Korea-based CHA Medical Group.
An adult-gerontology nurse practitioner (AGNP) is a nurse practitioner that specializes in continuing and comprehensive healthcare for adults across the lifespan from adolescence to old age.
This article describes disparities existing between men and women in accessing and receiving care for a stroke. This article also describes factors outside of the health care system which contribute to this disparity.

A mobile stroke unit(MSU) is an ambulance that furnishes services to diagnose, evaluate, and/or treat symptoms of an acute stroke. It may contain, in addition to the normal ambulance equipment, a device for brain imaging (computerized tomography), a point-of-care laboratory and telemedical interaction between ambulance and hospital (videoconferencing, exchange of videos of patient examination and CT scans). Thus, this specialized ambulance includes all the tools necessary for hyperacute assessment and treatment of stroke patients and diagnosis-based triage directly at the emergency site.

North Shore Medical Center (Miami) is a teaching hospital and a comprehensive stroke center in Miami, Florida. The hospital has more than 400 medical staff and over 700 employees. The hospital serves over 80,000 patients annually.
A cerebroprotectant is a drug that is intended to protect the brain after the onset of acute ischemic stroke. As stroke is the second largest cause of death worldwide and a leading cause of adult disability, over 150 drugs tested in clinical trials to provide cerebroprotection.
Opeolu Makanju Adeoye is an American physician who is the BJC HealthCare Distinguished Professor of Emergency Medicine and Department Chair at the Washington University School of Medicine. He was elected Fellow of the National Academy of Medicine in 2022.
Shyam K. Prabhakaran is an American vascular neurologist. He is the James Nelson and Anna Louise Raymond Professor and Chair of the Department of Neurology at the University of Chicago.