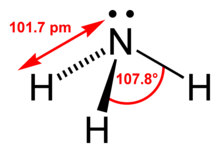
The urea breath test is a rapid diagnostic procedure used to identify infections by Helicobacter pylori, a spiral bacterium implicated in gastritis, gastric ulcer, and peptic ulcer disease. It is based upon the ability of H. pylori to convert urea to ammonia and carbon dioxide. Urea breath tests are recommended in leading society guidelines as a preferred non-invasive choice for detecting H. pylori before and after treatment.
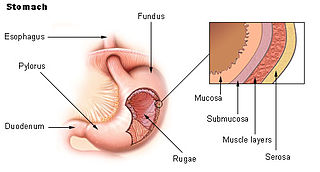
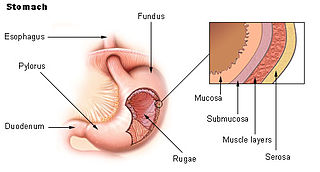
Peptic ulcer disease is a break in the inner lining of the stomach, the first part of the small intestine, or sometimes the lower esophagus. An ulcer in the stomach is called a gastric ulcer, while one in the first part of the intestines is a duodenal ulcer. The most common symptoms of a duodenal ulcer are waking at night with upper abdominal pain, and upper abdominal pain that improves with eating. With a gastric ulcer, the pain may worsen with eating. The pain is often described as a burning or dull ache. Other symptoms include belching, vomiting, weight loss, or poor appetite. About a third of older people with peptic ulcers have no symptoms. Complications may include bleeding, perforation, and blockage of the stomach. Bleeding occurs in as many as 15% of cases.
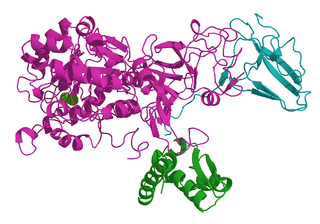
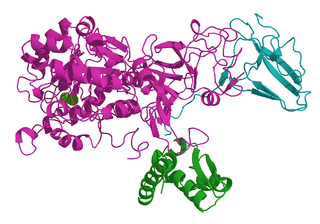
Ureases, functionally, belong to the superfamily of amidohydrolases and phosphotriesterases. Ureases are found in numerous bacteria, fungi, algae, plants, and some invertebrates, as well as in soils, as a soil enzyme. They are nickel-containing metalloenzymes of high molecular weight.

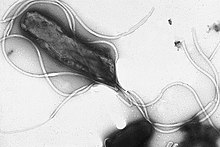
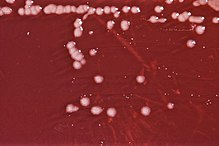
Helicobacter pylori, previously known as Campylobacter pylori, is a gram-negative, flagellated, helical bacterium. Mutants can have a rod or curved rod shape, and these are less effective. Its helical body is thought to have evolved in order to penetrate the mucous lining of the stomach, helped by its flagella, and thereby establish infection. The bacterium was first identified as the causal agent of gastric ulcers in 1983 by the Australian doctors Barry Marshall and Robin Warren.

Helicobacter is a genus of gram-negative bacteria possessing a characteristic helical shape. They were initially considered to be members of the genus Campylobacter, but in 1989, Goodwin et al. published sufficient reasons to justify the new genus name Helicobacter. The genus Helicobacter contains about 35 species.

Barry James Marshall is an Australian physician, Nobel Laureate in Physiology or Medicine, Professor of Clinical Microbiology and Co-Director of the Marshall Centre at the University of Western Australia. Marshall and Robin Warren showed that the bacterium Helicobacter pylori plays a major role in causing many peptic ulcers, challenging decades of medical doctrine holding that ulcers were caused primarily by stress, spicy foods, and too much acid. This discovery has allowed for a breakthrough in understanding a causative link between Helicobacter pylori infection and stomach cancer.

Gastritis is inflammation of the lining of the stomach. It may occur as a short episode or may be of a long duration. There may be no symptoms but, when symptoms are present, the most common is upper abdominal pain. Other possible symptoms include nausea and vomiting, bloating, loss of appetite and heartburn. Complications may include stomach bleeding, stomach ulcers, and stomach tumors. When due to autoimmune problems, low red blood cells due to not enough vitamin B12 may occur, a condition known as pernicious anemia.
Achlorhydria and hypochlorhydria refer to states where the production of hydrochloric acid in gastric secretions of the stomach and other digestive organs is absent or low, respectively. It is associated with various other medical problems.
Indigestion, also known as dyspepsia or upset stomach, is a condition of impaired digestion. Symptoms may include upper abdominal fullness, heartburn, nausea, belching, or upper abdominal pain. People may also experience feeling full earlier than expected when eating. Indigestion is relatively common, affecting 20% of people at some point during their life, and is frequently caused by gastroesophageal reflux disease (GERD) or gastritis.

A vagotomy is a surgical procedure that involves removing part of the vagus nerve. It is performed in the abdomen.
Helicobacter pylori eradication protocols is a standard name for all treatment protocols for peptic ulcers and gastritis in the presence of Helicobacter pylori infection. The primary goal of the treatment is not only temporary relief of symptoms but also total elimination of H. pylori infection. Patients with active duodenal or gastric ulcers and those with a prior ulcer history should be tested for H. pylori. Appropriate therapy should be given for eradication. Patients with MALT lymphoma should also be tested and treated for H. pylori since eradication of this infection can induce remission in many patients when the tumor is limited to the stomach. Several consensus conferences, including the Maastricht Consensus Report, recommend testing and treating several other groups of patients but there is limited evidence of benefit. This includes patients diagnosed with gastric adenocarcinoma, patients found to have atrophic gastritis or intestinal metaplasia, as well as first-degree relatives of patients with gastric adenocarcinoma since the relatives themselves are at increased risk of gastric cancer partly due to the intrafamilial transmission of H. pylori. To date, it remains controversial whether to test and treat all patients with functional dyspepsia, gastroesophageal reflux disease, or other non-GI disorders as well as asymptomatic individuals.

Stomach diseases include gastritis, gastroparesis, Crohn's disease and various cancers.

Troxipide is a drug used in the treatment of gastroesophageal reflux disease. Troxipide is a systemic non-antisecretory gastric cytoprotective agent with anti-ulcer, anti-inflammatory and mucus secreting properties irrespective of pH of stomach or duodenum. Troxipide is currently marketed in Japan (Aplace), China (Shuqi), South Korea (Defensa), and India (Troxip). It is used for the management of gastric ulcers, and amelioration of gastric mucosal lesions in acute gastritis and acute exacerbation of chronic gastritis.
Helicobacter felis is a bacterial species in the Helicobacteraceae family, Campylobacterales order, Helicobacter genus. This bacterium is Gram-negative, microaerophilic, urease-positive, and spiral-shaped. Its type strain is CS1T. It can be pathogenic.
Helicobacter salomonis is a species within the Helicobacter genus of Gram-negative bacteria. Helicobacter pylori is by far the best known Helicobacter species primarily because humans infected with it may develop gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers of the nonlymphoma type, and various subtypes of extranodal marginal zone lymphomass, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori is also associated with the development of bile duct cancer and has been associated with a wide range of other diseases, although its role in the development of many of these other diseases requires further study. Humans infected with H. salomonis may develop some of the same gastrointestinal diseases viz., stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers that are not lymphomas, and extranodal marginal B cell lymphomas of the stomach. Other non-H. pylori Helicobacter species that are known to be associated with these gastrointestinal diseases are Helicobacter bizzozeronii, Helicobacter suis, Helicobacter felis, and Helicobacter heilmannii s.s. Because of their disease associations, these four Helicobacter species plus H. salomonis are often group together and termed Helicobacter heilmannii sensu lato.
Acid peptic diseases, such as peptic ulcers, Zollinger-Ellison syndrome, and gastroesophageal reflux disease, are caused by distinct but overlapping pathogenic mechanisms involving acid effects on mucosal defense. Acid reflux damages the esophageal mucosa and may also cause laryngeal tissue injury, leading to the development of pulmonary symptoms.
Helicobacter heilmannii sensu lato refers to a group of bacterial species within the Helicobacter genus. The Helicobacter genus consists of at least 40 species of spiral-shaped flagellated, Gram-negative bacteria of which the by far most prominent and well-known species is Helicobacter pylori. H. pylori is associated with the development of gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers that are not lymphomas, and various subtypes of extranodal marginal zone lymphomas, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori has also been associated with the development of bile duct cancer and has been associated with a wide range of other diseases although its role in the development of many of these other diseases requires further study.
Helicobacter bizzozeronii is a species within the Helicobacter genus of Gram-negative bacteria. Helicobacter pylori is by far the best known Helicobacter species, primarily because humans infected with it may develop gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers of the nonlymphoma type, and various subtypes of extranodal marginal zone lymphomass, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori is also associated with the development of bile duct cancer and has been associated with a wide range of other diseases although its role in the development of many of these other diseases requires further study. Humans infected with H. bizzozeronii are prone to develop some of the same gastrointestinal diseases viz., stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers that are not lymphomas, and extranodal marginal B cell lymphomas of the stomach. Other non-H. pylori Helicobacter species that are known to be associated with these gastrointestinal diseases are Helicobacter felis, Helicobacter salomonis, Helicobacter suis, and Helicobacter heilmannii s.s. Because of their disease associations, these four Helicobacter species plus H. bizzozeronii are often grouped together and termed Helicobacter heilmannii sensu lato.
Helicobacter suis is a species within the Helicobacter genus of Gram-negative bacteria. Helicobacter pylori is by far the best known Helicobacter species, primarily because humans infected with it may develop gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers of the nonlymphoma type, and various subtypes of extranodal marginal zone lymphomass, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori is also associated with the development of bile duct cancer and has been associated with a wide range of other diseases although its role in the development of many of these other diseases requires further study. Humans infected with H. suis may develop some of the same gastrointestinal diseases - stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers that are not lymphomas, and extranodal marginal B cell lymphomas of the stomach. Other non-H. pylori Helicobacter species that are known to be associated with these gastrointestinal diseases are Helicobacter bizzozeronii, Helicobacter salomonis, Helicobacter felis, and Helicobacter heilmannii s.s. Because of their disease associations, these four Helicobacter species plus H. suis are often group together and termed Helicobacter heilmannii sensu lato.
Helicobacter heilmannii s.s. is a species within the Helicobacter genus of Gram negative bacteria. Helicobacter pylori is by far the best known Helicobacter species primarily because humans infected with it may develop gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers of the non-lymphoma type, and various subtypes of extranodal marginal zone lymphomass, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori is also associated with the development of bile duct cancer and has been associated with a wide range of other diseases although its role in the development of many of these other diseases requires further study. Humans infected with H. heilmannii s.s. may develop some of the same gastrointestinal diseases viz., stomach inflammation, stomach ulcers, duodenal ulcers, stomach cancers that are not lymphomas, and extranodal marginal B cell lymphomas of the stomach. Other non-H. pylori Helicobacter species that are known to be associated with these gastrointestinal diseases are Helicobacter bizzozeronii, Helicobacter suis, Helicobacter felis, and Helicobacter salomonis. Because of their disease associations, these four Helicobacter species plus H. heilmannii s.s. are often group together and termed Helicobacter heilmannii sensu lato.