Jaundice, also known as icterus, is a yellowish or greenish pigmentation of the skin and sclera due to high bilirubin levels. Jaundice in adults is typically a sign indicating the presence of underlying diseases involving abnormal heme metabolism, liver dysfunction, or biliary-tract obstruction. The prevalence of jaundice in adults is rare, while jaundice in babies is common, with an estimated 80% affected during their first week of life. The most commonly associated symptoms of jaundice are itchiness, pale feces, and dark urine.

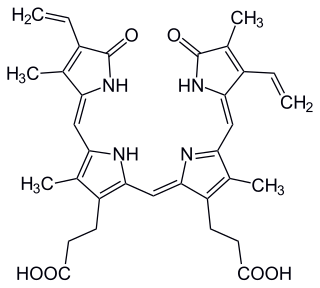
Bilirubin (BR) is a red-orange compound that occurs in the normal catabolic pathway that breaks down heme in vertebrates. This catabolism is a necessary process in the body's clearance of waste products that arise from the destruction of aged or abnormal red blood cells. In the first step of bilirubin synthesis, the heme molecule is stripped from the hemoglobin molecule. Heme then passes through various processes of porphyrin catabolism, which varies according to the region of the body in which the breakdown occurs. For example, the molecules excreted in the urine differ from those in the feces. The production of biliverdin from heme is the first major step in the catabolic pathway, after which the enzyme biliverdin reductase performs the second step, producing bilirubin from biliverdin.

Stercobilin is a tetrapyrrolic bile pigment and is one end-product of heme catabolism. It is the chemical responsible for the brown color of human feces and was originally isolated from feces in 1932. Stercobilin can be used as a marker for biochemical identification of fecal pollution levels in rivers.

Kernicterus is a bilirubin-induced brain dysfunction. The term was coined in 1904 by Christian Georg Schmorl. Bilirubin is a naturally occurring substance in the body of humans and many other animals, but it is neurotoxic when its concentration in the blood is too high, a condition known as hyperbilirubinemia. Hyperbilirubinemia may cause bilirubin to accumulate in the grey matter of the central nervous system, potentially causing irreversible neurological damage. Depending on the level of exposure, the effects range from clinically unnoticeable to severe brain damage and even death.

Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis fetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.

A bili light is a light therapy tool to treat newborn jaundice (hyperbilirubinemia). High levels of bilirubin can cause brain damage (kernicterus), leading to cerebral palsy, auditory neuropathy, gaze abnormalities and dental enamel hypoplasia. The therapy uses a blue light (420–470 nm) that converts bilirubin into an (E,Z)-isomer that can be excreted in the urine and feces. Soft goggles are put on the child to reduce eye damage from the high intensity light. The baby is kept naked or only wearing a diaper, and is turned over frequently to expose more of the skin.
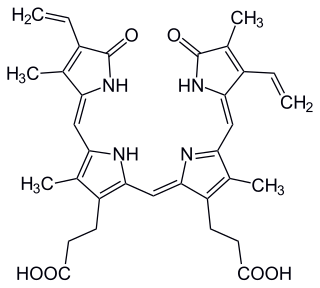
Biliverdin is a green tetrapyrrolic bile pigment, and is a product of heme catabolism. It is the pigment responsible for a greenish color sometimes seen in bruises.

Neonatal jaundice is a yellowish discoloration of the white part of the eyes and skin in a newborn baby due to high bilirubin levels. Other symptoms may include excess sleepiness or poor feeding. Complications may include seizures, cerebral palsy, or kernicterus.

Dubin–Johnson syndrome is a rare, autosomal recessive, benign disorder that causes an isolated increase of conjugated bilirubin in the serum. Classically, the condition causes a black liver due to the deposition of a pigment similar to melanin. This condition is associated with a defect in the ability of hepatocytes to secrete conjugated bilirubin into the bile, and is similar to Rotor syndrome. It is usually asymptomatic, but may be diagnosed in early infancy based on laboratory tests. No treatment is usually needed.

Crigler–Najjar syndrome is a rare inherited disorder affecting the metabolism of bilirubin, a chemical formed from the breakdown of the heme in red blood cells. The disorder results in a form of nonhemolytic jaundice, which results in high levels of unconjugated bilirubin and often leads to brain damage in infants. The disorder is inherited in an autosomal recessive manner. The annual incidence is estimated at 1 in 1,000,000.

HMOX1 is a human gene that encodes for the enzyme heme oxygenase 1. Heme oxygenase mediates the first step of heme catabolism, it cleaves heme to form biliverdin.

Heme oxygenase, or haem oxygenase, is an enzyme that catalyzes the degradation of heme to produce biliverdin, ferrous ion, and carbon monoxide.

Subgaleal hemorrhage, also known as subgaleal hematoma, is bleeding in the potential space between the skull periosteum and the scalp galea aponeurosis.

Biliverdin reductase (BVR) is an enzyme found in all tissues under normal conditions, but especially in reticulo-macrophages of the liver and spleen. BVR facilitates the conversion of biliverdin to bilirubin via the reduction of a double-bond between the second and third pyrrole ring into a single-bond.
In ABO hemolytic disease of the newborn maternal IgG antibodies with specificity for the ABO blood group system pass through the placenta to the fetal circulation where they can cause hemolysis of fetal red blood cells which can lead to fetal anemia and HDN. In contrast to Rh disease, about half of the cases of ABO HDN occur in a firstborn baby and ABO HDN does not become more severe after further pregnancies.
Neonatal cholestasis refers to elevated levels of conjugated bilirubin identified in newborn infants within the first few months of life. Conjugated hyperbilirubinemia is clinically defined as >20% of total serum bilirubin or conjugated bilirubin concentration greater than 1.0 mg/dL regardless of total serum bilirubin concentration. The differential diagnosis for neonatal cholestasis can vary extensively. However, the underlying disease pathology is caused by improper transport and/or defects in excretion of bile from hepatocytes leading to an accumulation of conjugated bilirubin in the body. Generally, symptoms associated with neonatal cholestasis can vary based on the underlying cause of the disease. However, most infants affected will present with jaundice, scleral icterus, failure to thrive, acholic or pale stools, and dark urine.

Heme oxygenase 2 is an enzyme that in humans is encoded by the HMOX2 gene.

Bilirubin glucuronide is a water-soluble reaction intermediate over the process of conjugation of indirect bilirubin. Bilirubin glucuronide itself belongs to the category of conjugated bilirubin along with bilirubin di-glucuronide. However, only the latter one is primarily excreted into the bile in the normal setting.
Hemolytic jaundice, also known as prehepatic jaundice, is a type of jaundice arising from hemolysis or excessive destruction of red blood cells, when the byproduct bilirubin is not excreted by the hepatic cells quickly enough. Unless the patient is concurrently affected by hepatic dysfunctions or is experiencing hepatocellular damage, the liver does not contribute to this type of jaundice.
Hyperbilirubinemia is a clinical condition describing an elevation of blood bilirubin level due to the inability to properly metabolise or excrete bilirubin, a product of erythrocytes breakdown. In severe cases, it is manifested as jaundice, the yellowing of tissues like skin and the sclera when excess bilirubin deposits in them. The US records 52,500 jaundice patients annually. By definition, bilirubin concentration of greater than 3 mg/ml is considered hyperbilirubinemia, following which jaundice progressively develops and becomes apparent when plasma levels reach 20 mg/ml. Rather than a disease itself, hyperbilirubinemia is indicative of multifactorial underlying disorders that trace back to deviations from regular bilirubin metabolism. Diagnosis of hyperbilirubinemia depends on physical examination, urinalysis, serum tests, medical history and imaging to identify the cause. Genetic diseases, alcohol, pregnancy and hepatitis viruses affect the likelihood of hyperbilirubinemia. Causes of hyperbilirubinemia mainly arise from the liver. These include haemolytic anaemias, enzymatic disorders, liver damage and gallstones. Hyperbilirubinemia itself is often benign. Only in extreme cases does kernicterus, a type of brain injury, occur. Therapy for adult hyperbilirubinemia targets the underlying diseases but patients with jaundice often have poor outcomes.