Related Research Articles

Endocytosis is a cellular process in which substances are brought into the cell. The material to be internalized is surrounded by an area of cell membrane, which then buds off inside the cell to form a vesicle containing the ingested material. Endocytosis includes pinocytosis and phagocytosis. It is a form of active transport.

The blood–brain barrier (BBB) is a highly selective semipermeable border of endothelial cells that prevents solutes in the circulating blood from non-selectively crossing into the extracellular fluid of the central nervous system where neurons reside. The blood–brain barrier is formed by endothelial cells of the capillary wall, astrocyte end-feet ensheathing the capillary, and pericytes embedded in the capillary basement membrane. This system allows the passage of some small molecules by passive diffusion, as well as the selective and active transport of various nutrients, ions, organic anions, and macromolecules such as glucose and amino acids that are crucial to neural function.
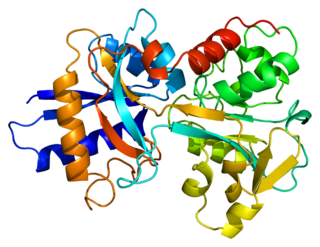
Transferrins are glycoproteins found in vertebrates which bind to and consequently mediate the transport of iron (Fe) through blood plasma. They are produced in the liver and contain binding sites for two Fe3+ ions. Human transferrin is encoded by the TF gene and produced as a 76 kDa glycoprotein.

Endosomes are a collection of intracellular sorting organelles in eukaryotic cells. They are parts of endocytic membrane transport pathway originating from the trans Golgi network. Molecules or ligands internalized from the plasma membrane can follow this pathway all the way to lysosomes for degradation or can be recycled back to the cell membrane in the endocytic cycle. Molecules are also transported to endosomes from the trans Golgi network and either continue to lysosomes or recycle back to the Golgi apparatus.
Protease-activated receptors(PAR) are a subfamily of related G protein-coupled receptors that are activated by cleavage of part of their extracellular domain. They are highly expressed in platelets, and also on endothelial cells, myocytes and neurons.
Intestinal permeability is a term describing the control of material passing from inside the gastrointestinal tract through the cells lining the gut wall, into the rest of the body. The intestine normally exhibits some permeability, which allows nutrients to pass through the gut, while also maintaining a barrier function to keep potentially harmful substances from leaving the intestine and migrating to the body more widely. In a healthy human intestine, small particles can migrate through tight junction claudin pore pathways, and particles up to 10–15 Å can transit through the paracellular space uptake route. There is some evidence abnormally increased intestinal permeability may play a role in some chronic diseases and inflammatory conditions. The most well understood condition with observed increased intestinal permeability is celiac disease.
Microfold cells are found in the gut-associated lymphoid tissue (GALT) of the Peyer's patches in the small intestine, and in the mucosa-associated lymphoid tissue (MALT) of other parts of the gastrointestinal tract. These cells are known to initiate mucosal immunity responses on the apical membrane of the M cells and allow for transport of microbes and particles across the epithelial cell layer from the gut lumen to the lamina propria where interactions with immune cells can take place.

Transferrin receptor (TfR) is a carrier protein for transferrin. It is needed for the import of iron into the cell and is regulated in response to intracellular iron concentration. It imports iron by internalizing the transferrin-iron complex through receptor-mediated endocytosis. The existence of a receptor for transferrin iron uptake had been recognized over half a century back. Earlier two transferrin receptors in humans, transferrin receptor 1 and transferrin receptor 2 had been characterized and until recently cellular iron uptake was believed to occur chiefly via these two well documented transferrin receptors. Both these receptors are transmembrane glycoproteins. TfR1 is a high affinity ubiquitously expressed receptor while expression of TfR2 is restricted to certain cell types and is unaffected by intracellular iron concentrations. TfR2 binds to transferrin with a 25-30 fold lower affinity than TfR1. Although TfR1 mediated iron uptake is the major pathway for iron acquisition by most cells and especially developing erythrocytes, several studies have indicated that the uptake mechanism varies depending upon the cell type. It is also reported that Tf uptake exists independent of these TfRs although the mechanisms are not well characterized. The multifunctional glycolytic enzyme glyceraldehyde 3-phosphate dehydrogenase has been shown to utilize post translational modifications to exhibit higher order moonlighting behavior wherein it switches its function as a holo or apo transferrin receptor leading to either iron delivery or iron export respectively.
The neonatal Fc receptor is a protein that in humans is encoded by the FCGRT gene. It is an IgG Fc receptor which is similar in structure to the MHC class I molecule and also associates with beta-2-microglobulin. In rodents, FcRn was originally identified as the receptor that transports maternal immunoglobulin G (IgG) from mother to neonatal offspring via mother's milk, leading to its name as the neonatal Fc receptor. In humans, FcRn is present in the placenta where it transports mother's IgG to the growing fetus. FcRn has also been shown to play a role in regulating IgG and serum albumin turnover. Neonatal Fc receptor expression is up-regulated by the proinflammatory cytokine, TNF-α, and down-regulated by IFN-γ.

The secretory component is a component of immunoglobulin A (IgA). Secretory component is a proteolytic cleavage product of the polymeric immunoglobulin receptor which remains associated with dimeric IgA in sero-mucus secretions. Polymeric IgA binds to the polymeric immunoglobulin receptor on the basolateral surface of epithelial cells and is taken up into the cell via transcytosis. The receptor-IgA complex passes through the cellular compartments before being secreted on the luminal surface of the epithelial cells, still attached to the receptor. Proteolysis of the receptor occurs and the dimeric IgA molecule, along with the secretory component, are free to diffuse throughout the lumen.

Cadherin 5, type 2 or VE-cadherin also known as CD144, is a type of cadherin. It is encoded by the human gene CDH5.

Transferrin receptor protein 1 (TfR1), also known as Cluster of Differentiation 71 (CD71), is a protein that in humans is encoded by the TFRC gene. TfR1 is required for iron import from transferrin into cells by endocytosis.

The intestinal epithelium is the single cell layer that form the luminal surface (lining) of both the small and large intestine (colon) of the gastrointestinal tract. Composed of simple columnar epithelial cells, it serves two main functions: absorbing useful substances into the body and restricting the entry of harmful substances. As part of its protective role, the intestinal epithelium forms an important component of the intestinal mucosal barrier. Certain diseases and conditions are caused by functional defects in the intestinal epithelium. On the other hand, various diseases and conditions can lead to its dysfunction which, in turn, can lead to further complications.

Paclitaxel trevatide is an experimental chemotherapy drug that is under development by Angiochem Inc, a Canadian biotech company. Phase II clinical trials have completed for several indications, and the company is preparing for phase III trials.

Cytosis is a transport mechanism for the movement of large quantities of molecules into and out of cells.
Transcellular transport involves the transportation of solutes by a cell through a cell. Transcellular transport can occur in three different ways active transport, passive transport, and transcytosis.

A nanoparticle–biomolecule conjugate is a nanoparticle with biomolecules attached to its surface. Nanoparticles are minuscule particles, typically measured in nanometers (nm), that are used in nanobiotechnology to explore the functions of biomolecules. Properties of the ultrafine particles are characterized by the components on their surfaces more so than larger structures, such as cells, due to large surface area-to-volume ratios. Large surface area-to-volume-ratios of nanoparticles optimize the potential for interactions with biomolecules.
Nanoparticles for drug delivery to the brain is a method for transporting drug molecules across the blood–brain barrier (BBB) using nanoparticles. These drugs cross the BBB and deliver pharmaceuticals to the brain for therapeutic treatment of neurological disorders. These disorders include Parkinson's disease, Alzheimer's disease, schizophrenia, depression, and brain tumors. Part of the difficulty in finding cures for these central nervous system (CNS) disorders is that there is yet no truly efficient delivery method for drugs to cross the BBB. Antibiotics, antineoplastic agents, and a variety of CNS-active drugs, especially neuropeptides, are a few examples of molecules that cannot pass the BBB alone. With the aid of nanoparticle delivery systems, however, studies have shown that some drugs can now cross the BBB, and even exhibit lower toxicity and decrease adverse effects throughout the body. Toxicity is an important concept for pharmacology because high toxicity levels in the body could be detrimental to the patient by affecting other organs and disrupting their function. Further, the BBB is not the only physiological barrier for drug delivery to the brain. Other biological factors influence how drugs are transported throughout the body and how they target specific locations for action. Some of these pathophysiological factors include blood flow alterations, edema and increased intracranial pressure, metabolic perturbations, and altered gene expression and protein synthesis. Though there exist many obstacles that make developing a robust delivery system difficult, nanoparticles provide a promising mechanism for drug transport to the CNS.
The blood-spinal cord barrier (BSCB) is a semipermeable anatomical interface that consists of the specialized small blood vessels that surround the spinal cord. While similar to the blood-brain barrier in function and morphology, it is physiologically independent and has several distinct characteristics. The BSCB is involved in many disorders affecting the central nervous system, including neurodegenerative diseases, pain disorders, and traumatic spinal cord injury. In conjunction with the blood-brain barrier, the BSCB contributes to the difficulty in delivering drugs to the central nervous system, which makes drug targeting of the BSCB an important goal in pharmaceutical research.

Focused ultrasound for intracrainial drug delivery is a non-invasive technique that uses high-frequency sound waves to disrupt tight junctions in the blood-brain barrier (BBB), allowing for increased passage of therapeutics into the brain. The BBB normally blocks nearly 98% of drugs from accessing the central nervous system, so FUS has the potential to address a major challenge in intracranial drug delivery by providing targeted and reversible BBB disruption. Using FUS to enhance drug delivery to the brain could significantly improve patient outcomes for a variety of diseases including Alzheimer's disease, Parkinson's disease, and brain cancer.
References
- ↑ "cytopempsis". The Free Dictionary.
- ↑ Perez, J. H.; Branch, W. J.; Smith, L.; Mullock, B. M.; Luzio, J. P. (1988). "Investigation of endosomal compartments involved in endocytosis and transcytosis of polymeric immunoglobulin a by subcellular fractionation of perfused isolated rat liver". The Biochemical Journal. 251 (3): 763–770. doi:10.1042/bj2510763. PMC 1149069 . PMID 3415644.
- ↑ Fishman, J. B.; Rubin, J. B.; Handrahan, J. V.; Connor, J. R.; Fine, R. E. (1987). "Receptor-mediated transcytosis of transferrin across the blood-brain barrier". Journal of Neuroscience Research. 18 (2): 299–304. doi:10.1002/jnr.490180206. PMID 3694713. S2CID 37435066.
- ↑ Duffy, K. R.; Pardridge, W. M. (1987). "Blood-brain barrier transcytosis of insulin in developing rabbits". Brain Research. 420 (1): 32–38. doi:10.1016/0006-8993(87)90236-8. PMID 3315116. S2CID 20376106.
- ↑ Williams, S. K.; Greener, D. A.; Solenski, N. J. (1984). "Endocytosis and exocytosis of protein in capillary endothelium". Journal of Cellular Physiology. 120 (2): 157–162. doi:10.1002/jcp.1041200208. PMID 6430919. S2CID 24779404.
- ↑ Fabian, R. H. (1991). "Retrograde axonal transport and transcytosis of immunoglobulins: Implications for the pathogenesis of autoimmune motor neuron disease". Advances in Neurology. 56: 433–444. PMID 1853776.
- ↑ Salo, J.; Lehenkari, P.; Mulari, M.; Metsikkö, K.; Väänänen, H. K. (1997). "Removal of osteoclast bone resorption products by transcytosis". Science. 276 (5310): 270–273. doi:10.1126/science.276.5310.270. PMID 9092479.
- ↑ Landsverk, T. (1987). "The follicle-associated epithelium of the ileal Peyer's patch in ruminants is distinguished by its shedding of 50 nm particles". Immunology and Cell Biology. 65 (3): 251–261. doi:10.1038/icb.1987.28. PMID 3623609. S2CID 22439008.
- ↑ Taub, M. E.; Shen, W. C. (1993). "Regulation of pathways within cultured epithelial cells for the transcytosis of a basal membrane-bound peroxidase-polylysine conjugate". Journal of Cell Science. 106 (4): 1313–1321. doi:10.1242/jcs.106.4.1313. PMID 8126110.
- ↑ Hunziker, W.; Peters, P. J. (1998). "Rab17 localizes to recycling endosomes and regulates receptor-mediated transcytosis in epithelial cells". The Journal of Biological Chemistry. 273 (25): 15734–15741. doi: 10.1074/jbc.273.25.15734 . PMID 9624171.
- ↑ Casanova, J. E.; Wang, X.; Kumar, R.; Bhartur, S. G.; Navarre, J.; Woodrum, J. E.; Altschuler, Y.; Ray, G. S.; Goldenring, J. R. (1999). "Association of Rab25 and Rab11a with the Apical Recycling System of Polarized Madin–Darby Canine Kidney Cells". Molecular Biology of the Cell. 10 (1): 47–61. doi:10.1091/mbc.10.1.47. PMC 25153 . PMID 9880326.
- ↑ Su, T.; Bryant, D. M.; Luton, F. D. R.; Vergés, M.; Ulrich, S. M.; Hansen, K. C.; Datta, A.; Eastburn, D. J.; Burlingame, A. L.; Shokat, K. M.; Mostov, K. E. (2010). "A kinase cascade leading to Rab11-FIP5 controls transcytosis of the polymeric immunoglobulin receptor". Nature Cell Biology. 12 (12): 1143–1153. doi:10.1038/ncb2118. PMC 3072784 . PMID 21037565.
- ↑ Rosato, R.; Jammes, H.; Belair, L.; Puissant, C.; Kraehenbuhl, J. P.; Djiane, J. (1995). "Polymeric-Ig receptor gene expression in rabbit mammary gland during pregnancy and lactation: Evolution and hormonal regulation". Molecular and Cellular Endocrinology. 110 (1–2): 81–87. doi:10.1016/0303-7207(95)03519-d. PMID 7672455. S2CID 10960352.
- ↑ Sun, Y.; Hu, G.; Zhang, X.; Minshall, R. D. (2009). "Phosphorylation of caveolin-1 regulates oxidant-induced pulmonary vascular permeability via paracellular and transcellular pathways". Circulation Research. 105 (7): 676–685, 15 685 following 685. doi:10.1161/CIRCRESAHA.109.201673. PMC 2776728 . PMID 19713536.
- ↑ Giri, C. P.; Shima, K.; Tall, B. D.; Curtis, S.; Sathyamoorthy, V.; Hanisch, B.; Kim, K. S.; Kopecko, D. J. (2011). "Cronobacter spp. (previously Enterobacter sakazakii) invade and translocate across both cultured human intestinal epithelial cells and human brain microvascular endothelial cells". Microbial Pathogenesis. 52 (2): 140–7. doi:10.1016/j.micpath.2011.10.003. PMID 22023990.
- ↑ Nikitas, G.; Deschamps, C.; Disson, O.; Niault, T.; Cossart, P.; Lecuit, M. (2011). "Transcytosis of Listeria monocytogenes across the intestinal barrier upon specific targeting of goblet cell accessible E-cadherin". Journal of Experimental Medicine. 208 (11): 2263–2277. doi:10.1084/jem.20110560. PMC 3201198 . PMID 21967767.
- ↑ Lukyanenko, V.; Malyukova, I.; Hubbard, A.; Delannoy, M.; Boedeker, E.; Zhu, C.; Cebotaru, L.; Kovbasnjuk, O. (2011). "Enterohemorrhagic Escherichia coli infection stimulates Shiga toxin 1 macropinocytosis and transcytosis across intestinal epithelial cells". AJP: Cell Physiology. 301 (5): C1140–C1149. doi:10.1152/ajpcell.00036.2011. PMC 3213915 . PMID 21832249.
- ↑ Simionescu, N.; Simionescu, M. (1985). "Interactions of endogenous lipoproteins with capillary endothelium in spontaneously hyperlipoproteinemic rats". Microvascular Research. 30 (3): 314–332. doi:10.1016/0026-2862(85)90063-9. PMID 4088094.
- ↑ Pardridge, W.M. (1986). "Receptor-mediated peptide transport through the blood-brain barrier". Endocrine Reviews. 7 (3): 314–330. doi:10.1210/edrv-7-3-314. PMID 3017689.
- ↑ Brightman, M.W.; Reese, T.S. (1969). "Junctions between intimately apposed cell membranes in the vertebrate brain". Journal of Cell Biology. 40 (3): 648–677. doi:10.1083/jcb.40.3.648. PMC 2107650 . PMID 5765759.
- ↑ Bundgaard, M (1984). "The three-dimensional organization of tight junctions in a capillary endothelium revealed by serial-section electron microscopy". Journal of Ultrastructure Research. 88 (1): 1–17. doi:10.1016/s0022-5320(84)90177-1. PMID 6545375.
- ↑ Pardridge, W.M. (2007). "Drug targeting to the brain". Pharmaceutical Research. 24 (9): 1733–1744. doi:10.1007/s11095-007-9324-2. PMID 17554607. S2CID 845668.
- ↑ Pardridge, W.M.; Boado, R.J. (2012). Reengineering biopharmaceuticals for targeted delivery across the blood-brain barrier. Methods in Enzymology. Vol. 503. pp. 269–292. doi:10.1016/B978-0-12-396962-0.00011-2. ISBN 9780123969620. PMID 22230573.
- ↑ Yu, Y. Joy; et al. (2001). "Boosting Brain Uptake of a Therapeutic Antibody by Reducing Its Affinity for a Transcytosis Target". Science Translational Medicine. 3 (84): 84. doi:10.1126/scitranslmed.3002230. PMID 21613623. S2CID 34161824.