Vaccination is the administration of a vaccine to help the immune system develop immunity from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating the body's adaptive immunity, they help prevent sickness from an infectious disease. When a sufficiently large percentage of a population has been vaccinated, herd immunity results. Herd immunity protects those who may be immunocompromised and cannot get a vaccine because even a weakened version would harm them. The effectiveness of vaccination has been widely studied and verified. Vaccination is the most effective method of preventing infectious diseases; widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the elimination of diseases such as polio and tetanus from much of the world. However, some diseases, such as measles outbreaks in America, have seen rising cases due to relatively low vaccination rates in the 2010s – attributed, in part, to vaccine hesitancy. According to the World Health Organization, vaccination prevents 3.5–5 million deaths per year.

The MMR vaccine is a vaccine against measles, mumps, and rubella, abbreviated as MMR. The first dose is generally given to children around 9 months to 15 months of age, with a second dose at 15 months to 6 years of age, with at least four weeks between the doses. After two doses, 97% of people are protected against measles, 88% against mumps, and at least 97% against rubella. The vaccine is also recommended for those who do not have evidence of immunity, those with well-controlled HIV/AIDS, and within 72 hours of exposure to measles among those who are incompletely immunized. It is given by injection.

Rubella, also known as German measles or three-day measles, is an infection caused by the rubella virus. This disease is often mild, with half of people not realizing that they are infected. A rash may start around two weeks after exposure and last for three days. It usually starts on the face and spreads to the rest of the body. The rash is sometimes itchy and is not as bright as that of measles. Swollen lymph nodes are common and may last a few weeks. A fever, sore throat, and fatigue may also occur. Joint pain is common in adults. Complications may include bleeding problems, testicular swelling, encephalitis, and inflammation of nerves. Infection during early pregnancy may result in a miscarriage or a child born with congenital rubella syndrome (CRS). Symptoms of CRS manifest as problems with the eyes such as cataracts, deafness, as well as affecting the heart and brain. Problems are rare after the 20th week of pregnancy.

Immunization, or immunisation, is the process by which an individual's immune system becomes fortified against an infectious agent.

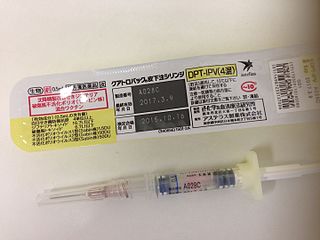
The DPT vaccine or DTP vaccine is a class of combination vaccines against three infectious diseases in humans: diphtheria, pertussis, and tetanus (lockjaw). The vaccine components include diphtheria and tetanus toxoids, and either killed whole cells of the bacterium that causes pertussis or pertussis antigens. The term toxoid refers to vaccines which use an inactivated toxin produced by the pathogen which they are targeted against to generate an immune response. In this way, the toxoid vaccine generates an immune response which is targeted against the toxin which is produced by the pathogen and causes disease, rather than a vaccine which is targeted against the pathogen itself. The whole cells or antigens will be depicted as either "DTwP" or "DTaP", where the lower-case "w" indicates whole-cell inactivated pertussis and the lower-case "a" stands for "acellular". In comparison to alternative vaccine types, such as live attenuated vaccines, the DTP vaccine does not contain any live pathogen, but rather uses inactivated toxoid to generate an immune response; therefore, there is not a risk of use in populations that are immune compromised since there is not any known risk of causing the disease itself. As a result, the DTP vaccine is considered a safe vaccine to use in anyone and it generates a much more targeted immune response specific for the pathogen of interest.
The MMRV vaccine combines the attenuated virus MMR vaccine with the addition of the varicella (chickenpox) vaccine. The MMRV vaccine is typically given to children between one and two years of age.

Mumps vaccines are vaccines which prevent mumps. When given to a majority of the population they decrease complications at the population level. Effectiveness when 90% of a population is vaccinated is estimated at 85%. Two doses are required for long term prevention. The initial dose is recommended between 12 and 18 months of age. The second dose is then typically given between two years and six years of age. Usage after exposure in those not already immune may be useful.
Immunization during pregnancy is the administration of a vaccine to a pregnant individual. This may be done either to protect the individual from disease or to induce an antibody response, such that the antibodies cross the placenta and provide passive immunity to the infant after birth. In many countries, including the US, Canada, UK, Australia and New Zealand, vaccination against influenza, COVID-19 and whooping cough is routinely offered during pregnancy.
The Expanded Program on Immunization(EPI) in the Philippines began in 1976 through Presidential Decree No. 996 signed by President Ferdinand Marcos. And, in 1986, made a response to the Universal Child Immunization goal. The four major strategies include:
- sustaining high routine Full Immunized Child (FIC) coverage of at least 90% in all provinces and cities;
- sustaining the polio-free country for global certification;
- eliminating measles by 2008; and
- eliminating neonatal tetanus by 2008.

Hepatitis B vaccine is a vaccine that prevents hepatitis B. The first dose is recommended within 24 hours of birth with either two or three more doses given after that. This includes those with poor immune function such as from HIV/AIDS and those born premature. It is also recommended that health-care workers be vaccinated. In healthy people, routine immunization results in more than 95% of people being protected.
A vaccination policy is a health policy adopted in order to prevent the spread of infectious disease. These policies are generally put into place by state or local governments, but may also be set by private facilities, such as workplaces or schools. Many policies have been developed and implemented since vaccines were first made widely available.
The Expanded Program on Immunization is a World Health Organization program with the goal to make vaccines available to all children.
Pertussis vaccine is a vaccine that protects against whooping cough (pertussis). There are two main types: whole-cell vaccines and acellular vaccines. The whole-cell vaccine is about 78% effective while the acellular vaccine is 71–85% effective. The effectiveness of the vaccines appears to decrease by between 2 and 10% per year after vaccination with a more rapid decrease with the acellular vaccines. The vaccine is only available in combination with tetanus and diphtheria vaccines. Pertussis vaccine is estimated to have saved over 500,000 lives in 2002.

Measles vaccine protects against becoming infected with measles. Nearly all of those who do not develop immunity after a single dose develop it after a second dose. When the rate of vaccination within a population is greater than 92%, outbreaks of measles typically no longer occur; however, they may occur again if the rate of vaccination decreases. The vaccine's effectiveness lasts many years. It is unclear if it becomes less effective over time. The vaccine may also protect against measles if given within a couple of days after exposure to measles.

Rubella vaccine is a vaccine used to prevent rubella. Effectiveness begins about two weeks after a single dose and around 95% of people become immune. Countries with high rates of immunization no longer see cases of rubella or congenital rubella syndrome. When there is a low level of childhood immunization in a population it is possible for rates of congenital rubella to increase as more women make it to child-bearing age without either vaccination or exposure to the disease. Therefore, it is important for more than 80% of people to be vaccinated. By introducing rubella containing vaccines, rubella has been eradicated in 81 nations, as of mid-2020.
A vaccine-preventable disease is an infectious disease for which an effective preventive vaccine exists. If a person acquires a vaccine-preventable disease and dies from it, the death is considered a vaccine-preventable death.
Tetanus vaccine, also known as tetanus toxoid (TT), is a toxoid vaccine used to prevent tetanus. During childhood, five doses are recommended, with a sixth given during adolescence.
Universal Immunisation Programme (UIP) is a vaccination programme launched by the Government of India in 1985. It became a part of Child Survival and Safe Motherhood Programme in 1992 and is currently one of the key areas under the National Health Mission since 2005. The programme now consists of vaccination for 12 diseases- tuberculosis, diphtheria, pertussis, tetanus, poliomyelitis, measles, hepatitis B, rotaviral gastroenteritis, Japanese encephalitis, rubella, pneumonia and Pneumococcal diseases. Hepatitis B and Pneumococcal diseases were added to the UIP in 2007 and 2017 respectively. The cost of all the vaccines are borne entirely by the Government of India and is funded through taxes with a budget of ₹7,234 crore (US$910 million) in 2022 and the program covers all residents of India, including foreign residents.

Mission Indradhanush is a health mission of the Government of India. It was launched by Union Health Minister J. P. Nadda on 25 December 2014. The scheme this seeks to drive towards 90% full immunisation coverage of India and sustain the same by year 2022. Vaccination is being provided against eight vaccine-preventable diseases nationally, i.e. Diphtheria, Whooping Cough, Tetanus, Polio, Measles, severe form of Childhood Tuberculosis and Hepatitis B and meningitis & pneumonia caused by Haemophilus influenza type B; and against Rotavirus Diarrhea and Japanese Encephalitis in selected states and districts respectively.

Vaccination policy of the United States is the subset of U.S. federal health policy that deals with immunization against infectious disease. It is decided at various levels of the government, including the individual states. This policy has been developed over the approximately two centuries since the invention of vaccination with the purpose of eradicating disease from the U.S. population, or creating a herd immunity. Policies intended to encourage vaccination impact numerous areas of law, including regulation of vaccine safety, funding of vaccination programs, vaccine mandates, adverse event reporting requirements, and compensation for injuries asserted to be associated with vaccination.