Related Research Articles
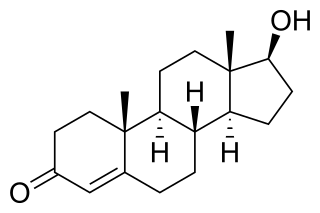
An androgen is any natural or synthetic steroid hormone that regulates the development and maintenance of male characteristics in vertebrates by binding to androgen receptors. This includes the embryological development of the primary male sex organs, and the development of male secondary sex characteristics at puberty. Androgens are synthesized in the testes, the ovaries, and the adrenal glands.
Hormone therapy or hormonal therapy is the use of hormones in medical treatment. Treatment with hormone antagonists may also be referred to as hormonal therapy or antihormone therapy. The most general classes of hormone therapy are oncologic hormone therapy, hormone replacement therapy, androgen replacement therapy (ART), oral contraceptive pills, and transgender hormone therapy.
Hypogonadism means diminished functional activity of the gonads—the testes or the ovaries—that may result in diminished production of sex hormones. Low androgen levels are referred to as hypoandrogenism and low estrogen as hypoestrogenism. These are responsible for the observed signs and symptoms in both males and females.

The history of intersex surgery is intertwined with the development of the specialities of pediatric surgery, pediatric urology, and pediatric endocrinology, with our increasingly refined understanding of sexual differentiation, with the development of political advocacy groups united by a human qualified analysis, and in the last decade by doubts as to efficacy, and controversy over when and even whether some procedures should be performed.

Leuprorelin, also known as leuprolide, is a manufactured version of a hormone used to treat prostate cancer, breast cancer, endometriosis, uterine fibroids, as part of transgender hormone therapy, for early puberty, or to perform chemical castration of violent sex offenders. It is given by injection into a muscle or under the skin.

Testosterone cypionate, sold under the brand name Depo-Testosterone among others, is an androgen and anabolic steroid (AAS) medication which is used mainly in the treatment of low testosterone levels in men. It is also used in hormone therapy for transgender men. It is given by injection into muscle or subcutaneously, once every one to four weeks, depending on clinical indication.

Testosterone enanthate is an androgen and anabolic steroid (AAS) medication which is used mainly in the treatment of low testosterone levels in men. It is also used in hormone therapy for transgender men. It is given by injection into muscle or subcutaneously usually once every one to four weeks.

Testosterone propionate, sold under the brand name Testoviron among others, is an androgen and anabolic steroid (AAS) medication which is used mainly in the treatment of low testosterone levels in men. It has also been used to treat breast cancer in women. It is given by injection into muscle usually once every two to three days.

Sexual differentiation in humans is the process of development of sex differences in humans. It is defined as the development of phenotypic structures consequent to the action of hormones produced following gonadal determination. Sexual differentiation includes development of different genitalia and the internal genital tracts and body hair plays a role in sex identification.
Pseudohermaphroditism is a condition in which an individual has a matching chromosomal and gonadal tissue sex, but mismatching external genitalia.

Disorders of sex development (DSDs), also known as differences in sex development, diverse sex development and variations in sex characteristics (VSC), are congenital conditions affecting the reproductive system, in which development of chromosomal, gonadal, or anatomical sex is atypical.
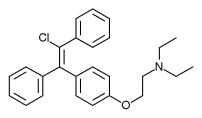
Enclomifene (INNTooltip International Nonproprietary Name), or enclomiphene (USANTooltip United States Adopted Name), a nonsteroidal selective estrogen receptor modulator of the triphenylethylene group acts by antagonizing the estrogen receptor (ER) in the pituitary gland, which reduces negative feedback by estrogen on the hypothalamic-pituitary-gonadal axis, thereby increasing gonadotropin secretion and hence gonadal production of testosterone. It is one of the two stereoisomers of clomifene, which itself is a mixture of 38% zuclomifene and 62% enclomifene. Enclomifene is the (E)-stereoisomer of clomifene, while zuclomifene is the (Z)-stereoisomer. Whereas zuclomifene is more estrogenic, enclomifene is more antiestrogenic. In accordance, unlike enclomifene, zuclomifene is antigonadotropic due to activation of the ER and reduces testosterone levels in men. As such, isomerically pure enclomifene is more favorable than clomifene as a progonadotropin for the treatment of male hypogonadism.
Masculinizing hormone therapy, also known as transmasculine hormone therapy, or female-to-male hormone therapy, is a form of hormone therapy and gender affirming therapy which is used to change the secondary sexual characteristics of transgender people from feminine or androgynous to masculine. It is a common type of transgender hormone therapy, and is predominantly used to treat transgender men and other transmasculine individuals. Some intersex people also receive this form of therapy, either starting in childhood to confirm the assigned sex or later if the assignment proves to be incorrect.
Feminizing hormone therapy, also known as transfeminine hormone therapy, is hormone therapy and sex reassignment therapy to change the secondary sex characteristics of transgender people from masculine or androgynous to feminine. It is a common type of transgender hormone therapy and is used to treat transgender women and non-binary transfeminine individuals. Some, in particular intersex people but also some non-transgender people, take this form of therapy according to their personal needs and preferences.

Intersex people are individuals born with any of several sex characteristics including chromosome patterns, gonads, or genitals that, according to the Office of the United Nations High Commissioner for Human Rights, "do not fit typical binary notions of male or female bodies".
Hypergonadotropic hypogonadism (HH), also known as primary or peripheral/gonadal hypogonadism or primary gonadal failure, is a condition which is characterized by hypogonadism which is due to an impaired response of the gonads to the gonadotropins, follicle-stimulating hormone (FSH) and luteinizing hormone (LH), and in turn a lack of sex steroid production. As compensation and the lack of negative feedback, gonadotropin levels are elevated. Individuals with HH have an intact and functioning hypothalamus and pituitary glands so they are still able to produce FSH and LH. HH may present as either congenital or acquired, but the majority of cases are of the former nature. HH can be treated with hormone replacement therapy.
Androgen deficiency is a medical condition characterized by insufficient androgenic activity in the body. Androgen deficiency most commonly affects women, and is also called Female androgen insufficiency syndrome (FAIS), although it can happen in both sexes. Androgenic activity is mediated by androgens, and is dependent on various factors including androgen receptor abundance, sensitivity and function. Androgen deficiency is associated with lack of energy and motivation, depression, lack of desire (libido), and in more severe cases changes in secondary sex characteristics.
Transgender hormone therapy, also called hormone replacement therapy (HRT) or gender-affirming hormone therapy (GAHT), is a form of hormone therapy in which sex hormones and other hormonal medications are administered to transgender or gender nonconforming individuals for the purpose of more closely aligning their secondary sexual characteristics with their gender identity. This form of hormone therapy is given as one of two types, based on whether the goal of treatment is masculinization or feminization:
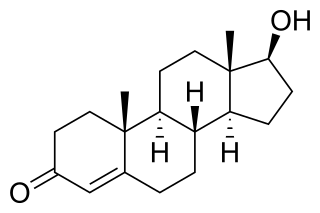
Testosterone (T) is a medication and naturally occurring steroid hormone. It is used to treat male hypogonadism, gender dysphoria, and certain types of breast cancer. It may also be used to increase athletic ability in the form of doping. It is unclear if the use of testosterone for low levels due to aging is beneficial or harmful. Testosterone can be used as a gel or patch that is applied to the skin, injection into a muscle, tablet that is placed in the cheek, or tablet that is taken by mouth.

The (DoDI) 6130.03, 2018, section 5, 13f and 14m is the writing which bars persons with "true hermaphroditism", "pseudohermaphroditism" and "pure gonadal dysgenesis" from serving in the United States Armed Forces. The three are all intersex conditions and are as of now considered to be medically incompatible with military service in the United States. "DoDI" stands for "Department of Defense Instruction," the 6130.03 instruction concerns "Medical Standards for Appointment, Enlistment, or Induction in the Military Services" in the Armed Forces of the United States. Section 5 focuses on disqualifying conditions of the male and female reproductive system, on the female page the subheader 13 and paragraph f name true hermaphroditism, pseudohermaphroditism and pure gonadal dysgenesis specifically, and on the male page the subheader 14 and paragraph m also name exactly true hermaphroditism, pseudohermaphroditism and pure gonadal dysgenesis, respectively. There is no differentiation made between males and females with these conditions. Many doctors, medical professionals and intersex advocates find the terms hermaphroditism to be outdated and stigmatized, therefore it and its derivative words are seldom used in the 2000s, with the word hermaphrodite itself being considered a slur when used against a human.
References
- ↑ "About the JH Clinical Research Network" . Retrieved October 29, 2021.
- ↑ "Adrian Sandra Dobs, M.D., M.H.S., Professor of Medicine". Johns Hopkins Medicine. Retrieved October 29, 2021.
- 1 2 3 "Adrian S. Dobs ICTR" . Retrieved October 29, 2021.
- ↑ "Dobs, Adrian Sandra - Author Detail". Scopus . Retrieved October 29, 2021.
- ↑ Dobs, Adrian S. (August 6, 2013). "A little better than placebo is still better than nothing". Nature Medicine. 19 (8): 962. doi: 10.1038/nm0813-962 . ISSN 1546-170X. PMID 23921736. S2CID 28045580.
- ↑ Squires, Sally (October 15, 1995). "FDA Approves Patch for Low Testosterone". Washington Post . Retrieved October 30, 2021.
- ↑ "The legal case of a Canadian athlete could change the way sports views gender". Newsweek. February 5, 2016. Retrieved October 30, 2021.
- ↑ "Lovingly, a family raises an intersex child - again". ABC News. Retrieved October 30, 2021.
- ↑ "Testosterone treatment shouldn't be given for aging, new guideline suggests". NBC News. January 7, 2020. Retrieved October 30, 2021.
- ↑ "Why It's Harder for Many Transgender People to Access (and Trust) COVID-19 Vaccines". Discover Magazine. Retrieved October 30, 2021.