Related Research Articles

Hepatitis is inflammation of the liver tissue. Some people or animals with hepatitis have no symptoms, whereas others develop yellow discoloration of the skin and whites of the eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pain, and diarrhea. Hepatitis is acute if it resolves within six months, and chronic if it lasts longer than six months. Acute hepatitis can resolve on its own, progress to chronic hepatitis, or (rarely) result in acute liver failure. Chronic hepatitis may progress to scarring of the liver (cirrhosis), liver failure, and liver cancer.

Hepatitis C is an infectious disease caused by the hepatitis C virus (HCV) that primarily affects the liver; it is a type of viral hepatitis. During the initial infection period, people often have mild or no symptoms. Early symptoms can include fever, dark urine, abdominal pain, and yellow tinged skin. The virus persists in the liver, becoming chronic, in about 70% of those initially infected. Early on, chronic infection typically has no symptoms. Over many years however, it often leads to liver disease and occasionally cirrhosis. In some cases, those with cirrhosis will develop serious complications such as liver failure, liver cancer, or dilated blood vessels in the esophagus and stomach.

Hepatology is the branch of medicine that incorporates the study of liver, gallbladder, biliary tree, and pancreas as well as management of their disorders. Although traditionally considered a sub-specialty of gastroenterology, rapid expansion has led in some countries to doctors specializing solely on this area, who are called hepatologists.

Alcoholic liver disease (ALD), also called alcohol-related liver disease (ARLD), is a term that encompasses the liver manifestations of alcohol overconsumption, including fatty liver, alcoholic hepatitis, and chronic hepatitis with liver fibrosis or cirrhosis.

Hepatotoxicity implies chemical-driven liver damage. Drug-induced liver injury is a cause of acute and chronic liver disease caused specifically by medications and the most common reason for a drug to be withdrawn from the market after approval.

Alcoholic hepatitis is hepatitis due to excessive intake of alcohol. Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8–10 drinks per day. It is usually found in association with fatty liver, an early stage of alcoholic liver disease, and may contribute to the progression of fibrosis, leading to cirrhosis. Symptoms may present acutely after a large amount of alcoholic intake in a short time period, or after years of excess alcohol intake. Signs and symptoms of alcoholic hepatitis include jaundice, ascites, fatigue and hepatic encephalopathy. Mild cases are self-limiting, but severe cases have a high risk of death. Severe cases may be treated with glucocorticoids. The condition often comes on suddenly and may progress in severity very rapidly.

Autoimmune hepatitis, formerly known as lupoid hepatitis, plasma cell hepatitis, or autoimmune chronic active hepatitis, is a chronic, autoimmune disease of the liver that occurs when the body's immune system attacks liver cells, causing the liver to be inflamed. Common initial symptoms may include fatigue, nausea, muscle aches, or weight loss or signs of acute liver inflammation including fever, jaundice, and right upper quadrant abdominal pain. Individuals with autoimmune hepatitis often have no initial symptoms and the disease may be detected by abnormal liver function tests and increased protein levels during routine bloodwork or the observation of an abnormal-looking liver during abdominal surgery.

Primary biliary cholangitis (PBC), previously known as primary biliary cirrhosis, is an autoimmune disease of the liver. It results from a slow, progressive destruction of the small bile ducts of the liver, causing bile and other toxins to build up in the liver, a condition called cholestasis. Further slow damage to the liver tissue can lead to scarring, fibrosis, and eventually cirrhosis.
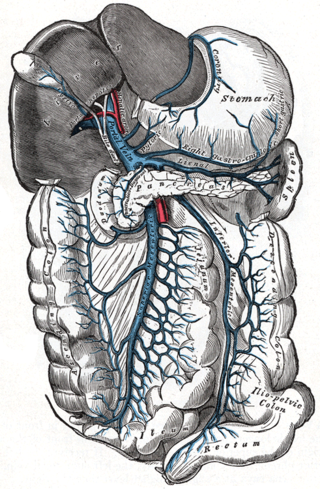
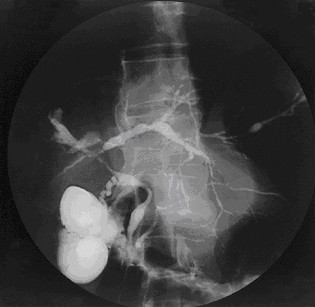
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg. Normal portal pressure is 1–4 mmHg; clinically insignificant portal hypertension is present at portal pressures 5–9 mmHg; clinically significant portal hypertension is present at portal pressures greater than 10 mmHg. The portal vein and its branches supply most of the blood and nutrients from the intestine to the liver.
Primary sclerosing cholangitis (PSC) is a long-term progressive disease of the liver and gallbladder characterized by inflammation and scarring of the bile ducts, which normally allow bile to drain from the gallbladder. Affected individuals may have no symptoms or may experience signs and symptoms of liver disease, such as yellow discoloration of the skin and eyes, itching, and abdominal pain.

Liver disease, or hepatic disease, is any of many diseases of the liver. If long-lasting it is termed chronic liver disease. Although the diseases differ in detail, liver diseases often have features in common.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

Hepatic encephalopathy (HE) is an altered level of consciousness as a result of liver failure. Its onset may be gradual or sudden. Other symptoms may include movement problems, changes in mood, or changes in personality. In the advanced stages it can result in a coma.

Acute liver failure is the appearance of severe complications rapidly after the first signs of liver disease, and indicates that the liver has sustained severe damage. The complications are hepatic encephalopathy and impaired protein synthesis. The 1993 classification defines hyperacute as within 1 week, acute as 8–28 days, and subacute as 4–12 weeks; both the speed with which the disease develops and the underlying cause strongly affect outcomes.
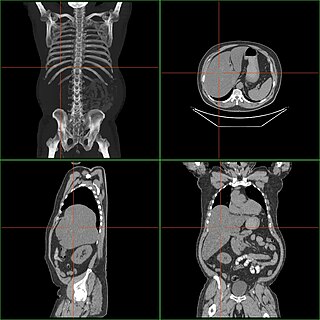
Hepatomegaly is enlargement of the liver. It is a non-specific medical sign, having many causes, which can broadly be broken down into infection, hepatic tumours, and metabolic disorder. Often, hepatomegaly presents as an abdominal mass. Depending on the cause, it may sometimes present along with jaundice.
The King's College Criteria or the King's College Hospital criteria were devised in 1989 to determine if there were any early indices of poor prognosis in patients with acute liver failure. Acute liver failure is defined as the onset of encephalopathy or coagulopathy within 26 weeks of a patient diagnosed with liver disease. Patients with hepatitis B acquired at birth, Wilson's disease and autoimmune hepatitis are included if their disease was identified within the past 26 weeks. These patients are very ill, and have a very high risk of dying of their illness without adequate treatment which may include liver transplantation. It is important that physicians find ways of identifying patients with acute liver failure early in their course who will do poorly, and may require liver transplantation. The King's College Criteria have consistently shown excellent operating characteristics for determining prognosis in these patients. As liver transplantation becomes a more accessible option for patients with acute liver failure, the King's College Criteria serve a role in determining which patients may require transplantation.

Liver failure is the inability of the liver to perform its normal synthetic and metabolic functions as part of normal physiology. Two forms are recognised, acute and chronic (cirrhosis). Recently, a third form of liver failure known as acute-on-chronic liver failure (ACLF) is increasingly being recognized.

Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage to the liver leads to repair of liver tissue and subsequent formation of scar tissue. Over time, scar tissue can replace normal functioning tissue, leading to the impaired liver function of cirrhosis. The disease typically develops slowly over months or years. Early symptoms may include tiredness, weakness, loss of appetite, unexplained weight loss, nausea and vomiting, and discomfort in the right upper quadrant of the abdomen. As the disease worsens, symptoms may include itchiness, swelling in the lower legs, fluid build-up in the abdomen, jaundice, bruising easily, and the development of spider-like blood vessels in the skin. The fluid build-up in the abdomen may develop into spontaneous infections. More serious complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus, stomach, or intestines, and liver cancer.
Hyperbilirubinemia is a clinical condition describing an elevation of blood bilirubin level due to the inability to properly metabolise or excrete bilirubin, a product of erythrocytes breakdown. In severe cases, it is manifested as jaundice, the yellowing of tissues like skin and the sclera when excess bilirubin deposits in them. The US records 52,500 jaundice patients annually. By definition, bilirubin concentration of greater than 3 mg/ml is considered hyperbilirubinemia, following which jaundice progressively develops and becomes apparent when plasma levels reach 20 mg/ml. Rather than a disease itself, hyperbilirubinemia is indicative of multifactorial underlying disorders that trace back to deviations from regular bilirubin metabolism. Diagnosis of hyperbilirubinemia depends on physical examination, urinalysis, serum tests, medical history and imaging to identify the cause. Genetic diseases, alcohol, pregnancy and hepatitis viruses affect the likelihood of hyperbilirubinemia. Causes of hyperbilirubinemia mainly arise from the liver. These include haemolytic anaemias, enzymatic disorders, liver damage and gallstones. Hyperbilirubinemia itself is often benign. Only in extreme cases does kernicterus, a type of brain injury, occur. Therapy for adult hyperbilirubinemia targets the underlying diseases but patients with jaundice often have poor outcomes.
References
- ↑ "NHS Choices". Cirrhosis. Retrieved 6 October 2015.
- ↑ Zetterman, Rowen. "Evaluating the Patient With Abnormal Liver Tests". Medscape. Retrieved 6 October 2015.
- 1 2 Chronic Liver Disease Causes, Symptoms And Treatment - 27/01/2007
- ↑ Liver Disease Archived 2010-01-31 at the Wayback Machine Gastro.com - 2007-01-27
- ↑ Liu ZL, Xie LZ, Zhu J, Li GQ, Grant SJ, Liu JP (2013). "Herbal medicines for fatty liver diseases". Cochrane Database Syst Rev. 8 (8): CD009059. doi: 10.1002/14651858.CD009059.pub2 . PMID 23975682.
- ↑ Green JL, Heard KJ, Reynolds KM, Albert D (2013). "Oral and Intravenous Acetylcysteine for Treatment of Acetaminophen Toxicity: A Systematic Review and Meta-analysis". Western Journal of Emergency Medicine. 14 (3): 218–226. doi: 10.5811/westjem.2012.4.6885 . PMC 3656701 . PMID 23687539.
- ↑ Montanini, S; Sinardi, D; Praticò, C; Sinardi, AU; Trimarchi, G (1999). "Use of acetylcysteine as the life-saving antidote in Amanita phalloides (death cap) poisoning". Arzneimittel-Forschung. 49 (12). National Institutes of Health: 1044–7. doi:10.1055/s-0031-1300549. PMID 10635453.
- ↑ Rainone, Francine (2005). "Milk Thistle". American Family Physician. 72 (7): 1285–8. PMID 16225032.
- ↑ "Liver disease: Alternative medicine". Mayo Clinic. 21 June 2023. Retrieved 1 January 2024.