Medicare is a government national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, but also for some younger people with disability status as determined by the SSA, including people with end stage renal disease and amyotrophic lateral sclerosis.

Patrick Joseph Tiberi is an American lobbyist and politician who served as the U.S. representative for Ohio's 12th congressional district from 2001 to 2018. His district included communities north and east of Columbus. He is a member of the Republican Party, and previously served in the Ohio House of Representatives from 1993 to 2000. He briefly served as Chair of the new Republican Main Street Congressional Caucus from September 7, 2017.

Medicare Part D, also called the Medicare prescription drug benefit, is an optional United States federal-government program to help Medicare beneficiaries pay for self-administered prescription drugs. Part D was enacted as part of the Medicare Modernization Act of 2003 and went into effect on January 1, 2006. Under the program, drug benefits are provided by private insurance plans that receive premiums from both enrollees and the government. Part D plans typically pay most of the cost for prescriptions filled by their enrollees. However, plans are later reimbursed for much of this cost through rebates paid by manufacturers and pharmacies.

The United States budget comprises the spending and revenues of the U.S. federal government. The budget is the financial representation of the priorities of the government, reflecting historical debates and competing economic philosophies. The government primarily spends on healthcare, retirement, and defense programs. The non-partisan Congressional Budget Office provides extensive analysis of the budget and its economic effects. It has reported that large budget deficits over the next 30 years are projected to drive federal debt held by the public to unprecedented levels—from 98 percent of gross domestic product (GDP) in 2020 to 195 percent by 2050.
Health care prices in the United States of America describes market and non-market factors that determine pricing, along with possible causes as to why prices are higher than other countries.
In the United States, health insurance helps pay for medical expenses through privately purchased insurance, social insurance, or a social welfare program funded by the government. Synonyms for this usage include "health coverage", "health care coverage", and "health benefits". In a more technical sense, the term "health insurance" is used to describe any form of insurance providing protection against the costs of medical services. This usage includes both private insurance programs and social insurance programs such as Medicare, which pools resources and spreads the financial risk associated with major medical expenses across the entire population to protect everyone, as well as social welfare programs like Medicaid and the Children's Health Insurance Program, which both provide assistance to people who cannot afford health coverage.

In the United States, health insurance coverage is provided by several public and private sources. During 2019, the U.S. population overall was approximately 330 million, with 59 million people 65 years of age and over covered by the federal Medicare program. The 273 million non-institutionalized persons under age 65 either obtained their coverage from employer-based or non-employer based sources, or were uninsured. During the year 2019, 89% of the non-institutionalized population had health insurance coverage. Separately, approximately 12 million military personnel received coverage through the Veteran's Administration and Military Health System.
In the United States, health insurance marketplaces, also called health exchanges, are organizations in each state through which people can purchase health insurance. People can purchase health insurance that complies with the Patient Protection and Affordable Care Act at ACA health exchanges, where they can choose from a range of government-regulated and standardized health care plans offered by the insurers participating in the exchange.
The healthcare reform debate in the United States has been a political issue focusing upon increasing medical coverage, decreasing costs, insurance reform, and the philosophy of its provision, funding, and government involvement.
There were a number of different health care reforms proposed during the Obama administration. Key reforms address cost and coverage and include obesity, prevention and treatment of chronic conditions, defensive medicine or tort reform, incentives that reward more care instead of better care, redundant payment systems, tax policy, rationing, a shortage of doctors and nurses, intervention vs. hospice, fraud, and use of imaging technology, among others.

The Affordable Care Act (ACA), formally known as the Patient Protection and Affordable Care Act and colloquially known as Obamacare, is a landmark U.S. federal statute enacted by the 111th United States Congress and signed into law by President Barack Obama on March 23, 2010. Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the enactment of Medicare and Medicaid in 1965.

The Path to Prosperity: Restoring America's Promise was the Republican Party's budget proposal for the federal government of the United States in the fiscal year 2012. It was succeeded in March 2012 by "The Path to Prosperity: A Blueprint for American Renewal", the Republican budget proposal for 2013. Representative Paul Ryan, Chairman of the House Budget Committee, played a prominent public role in drafting and promoting both The Path to Prosperity proposals, and they are therefore often referred to as the Ryan budget, Ryan plan or Ryan proposal.
Health care finance in the United States discusses how Americans obtain and pay for their healthcare, and why U.S. healthcare costs are the highest in the world based on various measures.
The Affordable Care Act (ACA) is divided into 10 titles and contains provisions that became effective immediately, 90 days after enactment, and six months after enactment, as well as provisions phased in through to 2020. Below are some of the key provisions of the ACA. For simplicity, the amendments in the Health Care and Education Reconciliation Act of 2010 are integrated into this timeline.

The economic policy of the Donald Trump administration was characterized by the individual and corporate tax cuts, attempts to repeal the Affordable Care Act ("Obamacare"), trade protectionism, immigration restriction, deregulation focused on the energy and financial sectors, and responses to the COVID-19 pandemic.

The following is a list of plans which were considered to replace the Affordable Care Act during the Donald Trump administration. The plans were considered after the Republican Party gained a federal government trifecta in 2016. "Repeal and replace" has been a Republican slogan since March 2010 when the ACA was signed into law and had been adopted by former President Donald Trump.

The American Health Care Act of 2017 was a bill in the 115th United States Congress. The bill, which was passed by the United States House of Representatives but not by the United States Senate, would have partially repealed the Affordable Care Act (ACA).

The Executive Order Promoting Healthcare Choice and Competition, also known as the Trumpcare Executive Order, or Trumpcare, is an Executive Order signed by Donald Trump on October 12, 2017, which directs federal agencies to modify how the Patient Protection and Affordable Care Act of the Obama Administration is implemented. The order included a directive to federal agencies to end rules forbidding employers from using health reimbursement arrangements (HRAs) to pay individual insurance premiums.
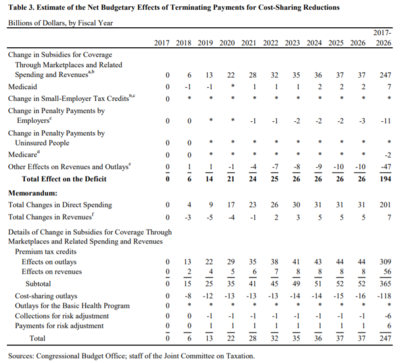
The Bipartisan Health Care Stabilization Act of 2017 was a 2017 proposed compromise reached by senator and HELP Committee chairman Lamar Alexander and senator and HELP Committee ranking member Patty Murray to amend the Affordable Care Act to fund cost-sharing reductions subsidies. The plan will also provide more flexibility for state waivers, allow a new "Copper Plan" or catastrophic coverage for those under 30, allow interstate insurance compacts, and redirect consumer fees to states for outreach. President Trump had stopped paying the cost sharing subsidies and the Congressional Budget Office estimated his action would cost $200 billion, cause insurance sold on the exchange to cost 20% more and cause one million people to lose insurance.
The Patient Protection and Affordable Care Act, often shortened to the Affordable Care Act (ACA) or nicknamed Obamacare, is a United States federal statute enacted by the 111th United States Congress and signed into law by President Barack Obama on March 23, 2010. Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the passage of Medicare and Medicaid in 1965. Once the law was signed, provisions began taking effect, in a process that continued for years. Some provisions never took effect, while others were deferred for various periods.