Radiation therapy or radiotherapy is a treatment using ionizing radiation, generally provided as part of cancer therapy to either kill or control the growth of malignant cells. It is normally delivered by a linear particle accelerator. Radiation therapy may be curative in a number of types of cancer if they are localized to one area of the body, and have not spread to other parts. It may also be used as part of adjuvant therapy, to prevent tumor recurrence after surgery to remove a primary malignant tumor. Radiation therapy is synergistic with chemotherapy, and has been used before, during, and after chemotherapy in susceptible cancers. The subspecialty of oncology concerned with radiotherapy is called radiation oncology. A physician who practices in this subspecialty is a radiation oncologist.

A brain tumor occurs when a group of cells within the brain turn cancerous and grow out of control, creating a mass. There are two main types of tumors: malignant (cancerous) tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

External beam radiation therapy (EBRT) is a form of radiotherapy that utilizes a high-energy collimated beam of ionizing radiation, from a source outside the body, to target and kill cancer cells. A radiotherapy beam is composed of particles which travel in a consistent direction; each radiotherapy beam consists of one type of particle intended for use in treatment, though most beams contain some contamination by other particle types.

A vestibular schwannoma (VS), also called acoustic neuroma, is a benign tumor that develops on the vestibulocochlear nerve that passes from the inner ear to the brain. The tumor originates when Schwann cells that form the insulating myelin sheath on the nerve malfunction. Normally, Schwann cells function beneficially to protect the nerves which transmit balance and sound information to the brain. However, sometimes a mutation in the tumor suppressor gene, NF2, located on chromosome 22, results in abnormal production of the cell protein named Merlin, and Schwann cells multiply to form a tumor. The tumor originates mostly on the vestibular division of the nerve rather than the cochlear division, but hearing as well as balance will be affected as the tumor enlarges.

Radiosurgery is surgery using radiation, that is, the destruction of precisely selected areas of tissue using ionizing radiation rather than excision with a blade. Like other forms of radiation therapy, it is usually used to treat cancer. Radiosurgery was originally defined by the Swedish neurosurgeon Lars Leksell as "a single high dose fraction of radiation, stereotactically directed to an intracranial region of interest".

Stereotactic surgery is a minimally invasive form of surgical intervention that makes use of a three-dimensional coordinate system to locate small targets inside the body and to perform on them some action such as ablation, biopsy, lesion, injection, stimulation, implantation, radiosurgery (SRS), etc.

Varian Medical Systems is an American radiation oncology treatments and software maker based in Palo Alto, California. Their medical devices include linear accelerators (LINACs) and software for treating cancer and other medical conditions with radiotherapy, radiosurgery, proton therapy, and brachytherapy. The company supplies software for managing cancer clinics, radiotherapy centers, and medical oncology practices. Varian Medical Systems employs more than 7,100 people at manufacturing sites in North America, Europe, and China and approximately 70 sites globally.
Elekta is a global Swedish company that develops and produces radiation therapy and radiosurgery-related equipment and clinical management for the treatment of cancer and brain disorders. Elekta has a global presence in more than 120 countries, with over 40 offices around the world and about 4,700 employees.
John R. Adler is an American neurosurgeon and medical device entrepreneur.

In radiotherapy, radiation treatment planning (RTP) is the process in which a team consisting of radiation oncologists, radiation therapist, medical physicists and medical dosimetrists plan the appropriate external beam radiotherapy or internal brachytherapy treatment technique for a patient with cancer.

Tomotherapy is a type of radiation therapy treatment machine. In tomotherapy a thin radiation beam is modulated as it rotates around the patient, while they are moved through the bore of the machine. The name comes from the use of a strip-shaped beam, so that only one “slice” of the target is exposed at any one time by the radiation. The external appearance of the system and movement of the radiation source and patient can be considered analogous to a CT scanner, which uses lower doses of radiation for imaging. Like a conventional machine used for X-ray external beam radiotherapy, it [the tomotherapy machine] generates the radiation beam, but the external appearance of the machine, patient positioning, and treatment delivery differ. Conventional linacs do not work on a slice-by-slice basis but typically have a large area beam which can also be resized and modulated.
Image-guided radiation therapy (IGRT) is the process of frequent imaging, during a course of radiation treatment, used to direct the treatment, position the patient, and compare to the pre-therapy imaging from the treatment plan. Immediately prior to, or during, a treatment fraction, the patient is localized in the treatment room in the same position as planned from the reference imaging dataset. An example of IGRT would include comparison of a cone beam computed tomography (CBCT) dataset, acquired on the treatment machine, with the computed tomography (CT) dataset from planning. IGRT would also include matching planar kilovoltage (kV) radiographs or megavoltage (MV) images with digital reconstructed radiographs (DRRs) from the planning CT.
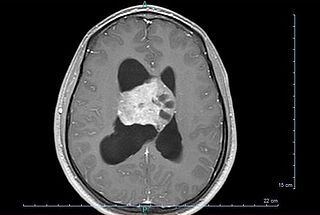
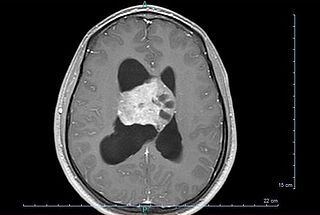
Central neurocytoma (CNC) is an extremely rare, ordinarily benign intraventricular brain tumour that typically forms from the neuronal cells of the septum pellucidum. The majority of central neurocytomas grow inwards into the ventricular system forming interventricular neurocytomas. This leads to two primary symptoms of CNCs, blurred vision and increased intracranial pressure. Treatment for a central neurocytoma typically involves surgical removal, with an approximate 1 in 5 chance of recurrence. Central neurocytomas are classified as a grade II tumor under the World Health Organization's classification of tumors of the nervous system.
James R. Doty, M.D., FACS, FICS, FAANS is a clinical professor of neurosurgery at Stanford University and founder and director of the Center for Compassion and Altruism Research and Education, an affiliate of the Stanford Neurosciences Institute. He is the author of a self-help book called Into the Magic Shop: A Neurosurgeon's Quest to Discover the Mysteries of the Brain and the Secrets of the Heart. Doty is also the Senior Editor of the Oxford Handbook of Compassion Science (2017).
Reno CyberKnife is a cancer treatment center in Reno, Nevada specializing in stereotactic radiosurgery. The center is a service of Saint Mary’s Regional Medical Center and is also a part of Saint Mary’s Brain Tumor Center. Reno CyberKnife is the only provider of CyberKnife technology in northern Nevada and frequently treats prostate and lung cancers and brain tumors.

Brainlab is a privately held German medical technology company headquartered in Munich, Bavaria. Brainlab develops software and hardware for radiotherapy and radiosurgery, and the surgical fields of neurosurgery, ENT and craniomaxillofacial, spine surgery, and traumatic interventions. Their products focus on image-guided surgery and radiosurgery, digital operating room integration technologies, and cloud-based data sharing. Brainlab is featured in the German media on topics such as the digitalisation of healthcare data and artificial intelligence in healthcare.

Jefferson Hospital for Neuroscience is a hospital in Center City Philadelphia, affiliated with Thomas Jefferson University and Thomas Jefferson University Hospital in Philadelphia. The hospital focuses on treating brain-related diseases and disorders. It is the only hospital of its kind in the Philadelphia area.

Jay Steven Loeffler was an American physician at Massachusetts General Hospital, where he served as chair of the Department of Radiation Oncology since 2000. He was the Herman and Joan Suit Professor of Radiation Oncology and professor of neurosurgery at Harvard Medical School.
Accuray is a radiation therapy company that develops, manufactures, and sells radiation therapy systems to deliver treatments including stereotactic radiosurgery (SRS) and stereotactic body radiation therapy (SBRT). It is the developer of innovative technologies, the CyberKnife and TomoTherapy platforms, including the Radixact System, the latest generation TomoTherapy platform. The company is headquartered in Sunnyvale, CA, the United States. The platforms are installed in leading healthcare centres in approximately 50 countries globally.
Surface-guided radiation therapy (SGRT) is the process of using 3D imaging to position and track movement of radiation therapy patients during treatment.