Related Research Articles

Caesarean section, also known as C-section or caesarean delivery, is the surgical procedure by which one or more babies are delivered through an incision in the mother's abdomen. It is often performed because vaginal delivery would put the mother or fetus at risk. Reasons for the operation include obstructed labor, twin pregnancy, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary.

Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically include abdominal pain and vaginal bleeding, but fewer than 50 percent of affected women have both of these symptoms. The pain may be described as sharp, dull, or crampy. Pain may also spread to the shoulder if bleeding into the abdomen has occurred. Severe bleeding may result in a fast heart rate, fainting, or shock. With very rare exceptions, the fetus is unable to survive.

Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In the developed countries, most deliveries occur in hospitals, while in the developing countries most are home births.

Misoprostol is a synthetic prostaglandin medication used to prevent and treat stomach and duodenal ulcers, induce labor, cause an abortion, and treat postpartum bleeding due to poor contraction of the uterus. It is taken by mouth when used to prevent gastric ulcers in people taking nonsteroidal anti-inflammatory drugs (NSAID). For abortions it is used by itself or in conjunction with mifepristone or methotrexate. By itself, effectiveness for abortion is between 66% and 90%. For labor induction or abortion, it is taken by mouth, dissolved in the mouth, or placed in the vagina. For postpartum bleeding it may also be used rectally.

Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening. Symptoms include vaginal bleeding in the second half of pregnancy. The bleeding is bright red and tends not to be associated with pain. Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery. Complications for the baby may include fetal growth restriction.

External cephalic version (ECV) is a process by which a breech baby can sometimes be turned from buttocks or foot first to head first. It is a manual procedure that is recommended by national guidelines for breech presentation of a pregnancy with a single baby, in order to enable vaginal delivery. It is usually performed late in pregnancy, that is, after 36 gestational weeks, preferably 37 weeks, and can even be performed in the early stages of childbirth.
Labor induction is the process or treatment that stimulates childbirth and delivery. Inducing (starting) labor can be accomplished with pharmaceutical or non-pharmaceutical methods. In Western countries, it is estimated that one-quarter of pregnant women have their labor medically induced with drug treatment. Inductions are most often performed either with prostaglandin drug treatment alone, or with a combination of prostaglandin and intravenous oxytocin treatment.
A hysterotomy is an incision made in the uterus. This surgical incision is used in several medical procedures, including during termination of pregnancy in the second trimester and delivering the fetus during caesarean section. It is also used to gain access and perform surgery on a fetus during pregnancy to correct birth defects, and it is an option to achieve resuscitation if cardiac arrest occurs during pregnancy and it is necessary to remove the fetus from the uterus.
Antepartum bleeding, also known as antepartum haemorrhage (APH) or prepartum hemorrhage, is genital bleeding during pregnancy after the 28th week of pregnancy up to delivery.
Cervical dilation is the opening of the cervix, the entrance to the uterus, during childbirth, miscarriage, induced abortion, or gynecological surgery. Cervical dilation may occur naturally, or may be induced surgically or medically.

Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth. Symptoms, while classically including increased pain, vaginal bleeding, or a change in contractions, are not always present. Disability or death of the mother or baby may result.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.
Caesarean delivery on maternal request (CDMR) is a caesarean section birth requested by the pregnant woman without a medical reason.
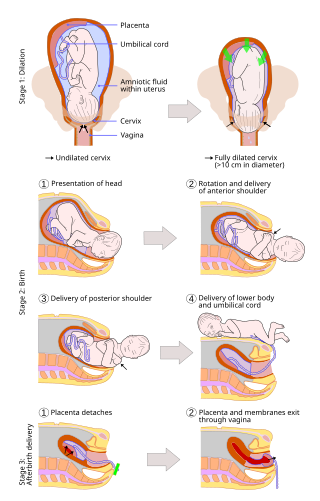
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, with lower morbidity and mortality than caesarean sections (C-sections).

Monoamniotic twins are identical or semi-identical twins that share the same amniotic sac within their mother's uterus. Monoamniotic twins are always monochorionic and are usually termed Monoamniotic-Monochorionic twins. They share the placenta, but have two separate umbilical cords. Monoamniotic twins develop when an embryo does not split until after formation of the amniotic sac, at about 9–13 days after fertilization. Monoamniotic triplets or other monoamniotic multiples are possible, but extremely rare. Other obscure possibilities include multiples sets where monoamniotic twins are part of a larger gestation such as triplets, quadruplets, or more.
The Human Microbiome Project (HMP), completed in 2012, laid the foundation for further investigation into the role the microbiome plays in overall health and disease. One area of particular interest is the role which delivery mode plays in the development of the infant/neonate microbiome and what potential implications this may have long term. It has been found that infants born via vaginal delivery have microbiomes closely mirroring that of the mother's vaginal microbiome, whereas those born via cesarean section tend to resemble that of the mother's skin. One notable study from 2010 illustrated an abundance of Lactobacillus and other typical vaginal genera in stool samples of infants born via vaginal delivery and an abundance of Staphylococcus and Corynebacterium, commonly found on the skin surfaces, in stool samples of infants born via cesarean section. From these discoveries came the concept of vaginal seeding, also known as microbirthing, which is a procedure whereby vaginal fluids are applied to a new-born child delivered by caesarean section. The idea of vaginal seeding was explored in 2015 after Maria Gloria Dominguez-Bello discovered that birth by caesarean section significantly altered the newborn child's microbiome compared to that of natural birth. The purpose of the technique is to recreate the natural transfer of bacteria that the baby gets during a vaginal birth. It involves placing swabs in the mother's vagina, and then wiping them onto the baby's face, mouth, eyes and skin. Due to the long-drawn nature of studying the impact of vaginal seeding, there are a limited number of studies available that support or refute its use. The evidence suggests that applying microbes from the mother's vaginal canal to the baby after cesarean section may aid in the partial restoration of the infant's natural gut microbiome with an increased likelihood of pathogenic infection to the child via vertical transmission.
Trial of labor after caesarean (TOLAC) is the term for an attempted birth in a patient who has had a previous caesarean section. It may result in a successful VBAC (vaginal birth after caesarean) or a repeat caesarean section. In approximately 20-40% of TOLACs, a caesarean is performed. TOLAC is recommended when a patient has had one previous caesarean section using a low transverse uterine incision. The main risks of TOLAC are emergency caesarean section and uterine rupture.

A uterine niche, also known as a Cesarean scar defect or an isthmocele, is an indentation of the myometrium at the site of a cesarean section with a depth of at least 2 mm.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 "Birth After Previous Caesarean Birth, Green-top Guideline No. 45" (PDF). Royal College of Obstetricians and Gynaecologists. February 2007. Archived from the original (PDF) on 2014-12-07.
- 1 2 "Vaginal Birth after Cesarean (VBAC)". American Pregnancy Association. Archived from the original on 2012-06-21. Retrieved 2012-06-16.
- 1 2 3 Vaginal birth after C-section (VBAC) guide, Mayo Clinic
- 1 2 3 4 5 American Congress of Obstetricians and, Gynecologists (Aug 2010). "ACOG Practice bulletin no. 115: Vaginal birth after previous cesarean delivery". Obstetrics and Gynecology. 116 (2 Pt 1): 450–63. doi:10.1097/AOG.0b013e3181eeb251. PMID 20664418.
- 1 2 3 4 5 "NIH Vaginal Birth After Cesarean (VBAC) Conference - Panel Statement". NIH Consensus Development Program. March 8–10, 2010. Retrieved 2012-06-16.
- ↑ "Vaginal Birth After Cesarean: New Insights: Structured Abstract". Ahrq.gov. 16 September 2010.
- ↑ "Page Not Found". www.acog.org. Archived from the original on July 23, 2010.
{{cite web}}: Cite uses generic title (help) - 1 2 3 "Maternal, Infant, and Child Health—Healthy People". Healthypeople.gov. 13 September 2012.
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK507844/
- ↑ "Guideline Synthesis: Vaginal Birth After Cesarean (VBAC)". National Guideline Clearinghouse. Archived from the original on 2012-03-20. Retrieved 2012-06-16.
- ↑ Lanneau, Grainger S.; Muffley, Patrick; Magann, Everett F. (2009). "Cesarean Birth: Surgical Techniques". The Global Library of Women's Medicine. doi:10.3843/GLOWM.10133. ISSN 1756-2228.
- 1 2 American Congress of Obstetricians and Gynecologists (ACOG). "Guideline on Vaginal birth after previous cesarean delivery: Major Recommendations". guideline.gov. Archived from the original on 2008-01-15. Retrieved 2008-02-09.
- ↑ ACOG Practice Bulletin Number 115, August 2010
- ↑ Queensland Maternity; Neonatal Clinical Guidelines Program (November 2009). "Queensland Maternity and Neonatal Clinical Guideline: Vaginal birth after caesarean section (VBAC)" (PDF). Archived from the original (PDF) on 30 April 2012. Retrieved 22 September 2012.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8032534/
- 1 2 3 "Vaginal Birth After Cesarean: New Insights". Agency for Healthcare Research and Quality. March 2010. Retrieved 2012-06-16.
- ↑ https://www.ontariomidwives.ca/sites/default/files/2017-06/Thinking-about-VBAC-English.pdf
- ↑ "NCHS Data Brief: Recent Trends in Cesarean Delivery in the United States Products". Centers for Disease Control and Prevention. March 2010. Retrieved 2012-06-16.
- ↑ "Cesarean births, repeat (percent)—Health Indicators Warehouse". Healthindicators.gov. Archived from the original on 2012-03-23. Retrieved 2011-08-15.
- ↑ "Rates for Total Cesarean Section, Primary Cesarean Section and Vaginal Birth After Cesarean Section (VBAC), United States, 1989–2006." Archived February 17, 2013, at the Wayback Machine Childbirth Connection Archived 2008-11-02 at the Wayback Machine , 2008. Retrieved 25 September 2008.
- ↑ McMahon MJ, Luther ER, Bowes WA, Olshan AF (1996). "Comparison of a Trial of Labor with an Elective Second Cesarean Section". New England Journal of Medicine. 335 (10): 689–695. doi: 10.1056/NEJM199609053351001 . PMID 8703167.
- ↑ "Vaginal Birth After Cesarean: New Insights: Structured Abstract". Ahrq.gov. 16 September 2010.
- ↑ "Page Not Found". www.acog.org. Archived from the original on July 23, 2010.
{{cite web}}: Cite uses generic title (help) - ↑ "Rates of Cesarean Delivery - United States, 1993". Centers for Disease Control and Prevention. Retrieved 2012-06-16.
- ↑ McMahon MJ, Luther ER, Bowes WA, Olshan AF (September 1996). "Comparison of a trial of labor with an elective second cesarean section". New England Journal of Medicine. 335 (10): 689–95. doi: 10.1056/NEJM199609053351001 . PMID 8703167.
- ↑ Int J Gyn Obs; 1999; vol 66, p. 197
- ↑ "Cesarean births, repeat (percent)". Health Indicators Warehouse. Archived from the original on 2012-03-23. Retrieved 2012-06-16.
- ↑ "ACOG - Ob Gyns Issue Less Restrictive VBAC Guidelines". Archived from the original on 2012-06-05. Retrieved 2012-07-23.
- ↑ "2020 Topics & Objectives: Maternal, Infant, and Child Health". U.S. Department of Health and Human Services. Retrieved 2012-06-16.
- ↑ American Congress of Obstetricians and Gynecologists (ACOG). "Guideline on Vaginal birth after previous cesarean delivery". guideline.gov. Archived from the original on 2008-01-15. Retrieved 2008-02-09.
- ↑ Zweifler J, Garza A, Hughes S, Stanich MA, Hierholzer A, Lau M (2006). "Vaginal birth after cesarean in California: before and after a change in guidelines". Ann Fam Med. 4 (3): 228–34. doi:10.1370/afm.544. PMC 1479438 . PMID 16735524.
- ↑ Rita Rubin (24 August 2005). "Battle lines drawn over C-sections". USA Today. Retrieved 2008-02-09.
- ↑ "Vaginal Birth After Cesarean Calculator". Agency for Healthcare Research and Quality. 2013-10-24. Retrieved 2013-07-10.
- ↑ Kennare R, Tucker G, Heard A, Chan A (2007). "Risks of adverse outcomes in the next birth after a first cesarean delivery". Obstet Gynecol. 109 (2 Pt 1): 270–6. doi:10.1097/01.AOG.0000250469.23047.73. PMID 17267823. S2CID 5101397.