Central pontine myelinolysis is a neurological condition involving severe damage to the myelin sheath of nerve cells in the pons. It is predominately iatrogenic (treatment-induced), and is characterized by acute paralysis, dysphagia, dysarthria, and other neurological symptoms.
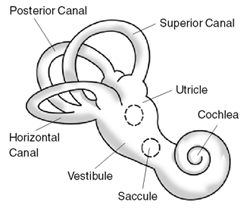
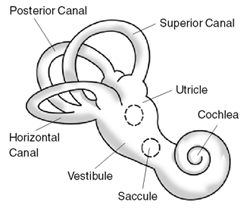
Ménière's disease (MD) is a disease of the inner ear that is characterized by potentially severe and incapacitating episodes of vertigo, tinnitus, hearing loss, and a feeling of fullness in the ear. Typically, only one ear is affected initially, but over time, both ears may become involved. Episodes generally last from 20 minutes to a few hours. The time between episodes varies. The hearing loss and ringing in the ears can become constant over time.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, death.
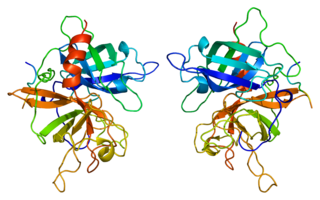
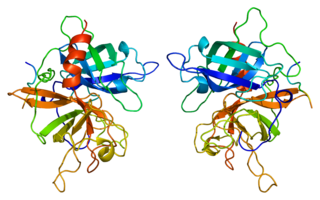
Tissue-type plasminogen activator, short name tPA, is a protein that facilitates the breakdown of blood clots. It acts as an enzyme to convert plasminogen into its active form plasmin, the major enzyme responsible for clot breakdown. It is a serine protease found on endothelial cells lining the blood vessels. Human tPA is encoded by the PLAT gene, and has a molecular weight of ~70 kDa in the single-chain form.

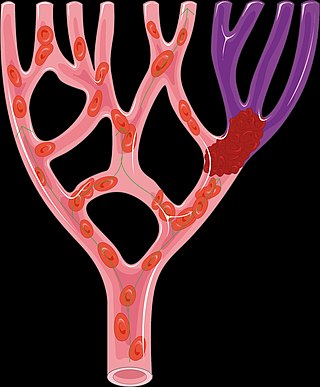
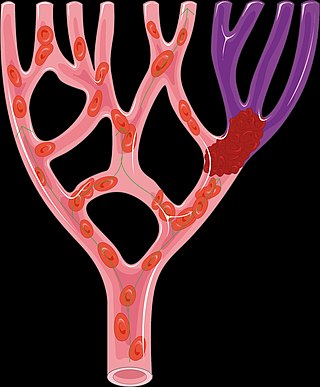
Stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functioning properly.

A glioma is a type of tumor that starts in the glial cells of the brain or the spine. Gliomas comprise about 30 percent of all brain tumors and central nervous system tumours, and 80 percent of all malignant brain tumours.
Alteplase, sold under the brand name Activase among others, is a biosynthetic form of human tissue-type plasminogen activator (t-PA). It is a thrombolytic medication used to treat acute ischemic stroke, acute ST-elevation myocardial infarction, pulmonary embolism associated with low blood pressure, and blocked central venous catheter. It is given by injection into a vein or artery. Alteplase is the same as the normal human plasminogen activator produced in vascular endothelial cells and is synthesized via recombinant DNA technology in Chinese hamster ovary cells (CHO). Alteplase causes the breakdown of a clot by inducing fibrinolysis.

Neuroprotection refers to the relative preservation of neuronal structure and/or function. In the case of an ongoing insult the relative preservation of neuronal integrity implies a reduction in the rate of neuronal loss over time, which can be expressed as a differential equation. It is a widely explored treatment option for many central nervous system (CNS) disorders including neurodegenerative diseases, stroke, traumatic brain injury, spinal cord injury, and acute management of neurotoxin consumption. Neuroprotection aims to prevent or slow disease progression and secondary injuries by halting or at least slowing the loss of neurons. Despite differences in symptoms or injuries associated with CNS disorders, many of the mechanisms behind neurodegeneration are the same. Common mechanisms of neuronal injury include decreased delivery of oxygen and glucose to the brain, energy failure, increased levels in oxidative stress, mitochondrial dysfunction, excitotoxicity, inflammatory changes, iron accumulation, and protein aggregation. Of these mechanisms, neuroprotective treatments often target oxidative stress and excitotoxicity—both of which are highly associated with CNS disorders. Not only can oxidative stress and excitotoxicity trigger neuron cell death but when combined they have synergistic effects that cause even more degradation than on their own. Thus limiting excitotoxicity and oxidative stress is a very important aspect of neuroprotection. Common neuroprotective treatments are glutamate antagonists and antioxidants, which aim to limit excitotoxicity and oxidative stress respectively.

Desmoteplase is a novel, highly fibrin-specific "clot-busting" (thrombolytic) drug in development that reached phase III clinical trials. The Danish pharmaceutical company, Lundbeck, owns the worldwide rights to Desmoteplase. In 2009, two large trials were started to test it as a safe and effective treatment for patients with acute ischaemic stroke. After disappointing results in DIAS-3, DIAS-4 was terminated, and in December 2014 Lundbeck announced that they would stop the development of desmoteplase.

Cerebral infarction is the pathologic process that results in an area of necrotic tissue in the brain. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia), most commonly due to thromboembolism, and manifests clinically as ischemic stroke. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.
Tenecteplase, sold under the trade names TNKase, Metalyse and Elaxim, is an enzyme used as a thrombolytic drug.
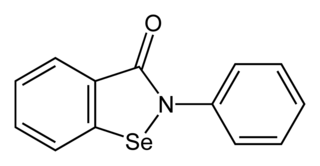
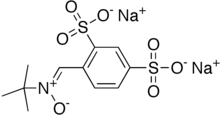
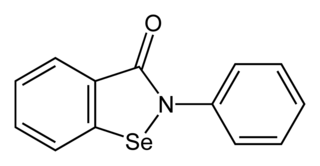
Ebselen, is a synthetic organoselenium drug molecule with anti-inflammatory, anti-oxidant and cytoprotective activity. It acts as a mimic of glutathione peroxidase and can also react with peroxynitrite. It is being investigated as a possible treatment for reperfusion injury and stroke, Ménière's disease, hearing loss and tinnitus, and bipolar disorder.

A brainstem glioma is a cancerous glioma tumor in the brainstem. Around 75% are diagnosed in children and young adults under the age of twenty, but have been known to affect older adults as well. Brainstem gliomas start in the brain or spinal cord tissue and typically spread throughout the nervous system.

Aptiganel is an unsuccessful drug candidate which acts as a noncompetitive NMDA antagonist, and that was under development by Cambridge Neuroscience, Inc as a treatment for stroke. It has neuroprotective effects and was researched for potential use in the treatment of stroke, but despite positive results in animal studies, human trials showed limited efficacy, as well as undesirable side effects such as sedation and hallucinations, and clinical development was ultimately not continued.

Lubeluzole (Prosynap) is a drug which acts as an indirect NMDA antagonist. It inhibits the release of glutamate, inhibits nitric oxide synthesis, and blocks calcium and sodium gated ion channels. It has neuroprotective effects particularly in hypoxic conditions, and was developed for the treatment of stroke. Trials showed it to be safe, effective and well tolerated at low doses, but unfortunately higher doses produced the dangerous cardiac side effect of lengthening the QTc interval, which could potentially lead to heart failure, and so this meant that subsequent trials were limited to using only the low dose range. Animal studies had shown lubeluzole to produce neuroprotective effects when administered for prolonged periods, but the aim of its developers was to produce a drug that would be effective for preventing damage from acute stroke, and so ultimately it failed to show sufficient efficacy in trials and development for medical use was halted.
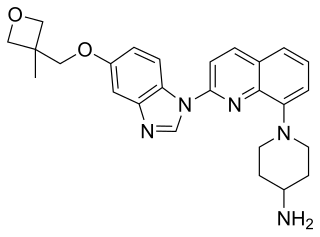
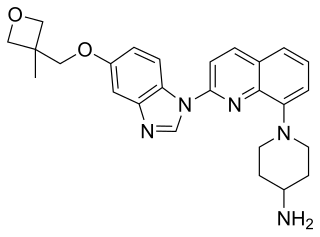
Crenolanib besylate is an investigational inhibitor being developed by AROG Pharmaceuticals, LLC. The compound is currently being evaluated for safety and efficacy in clinical trials for various types of cancer, including acute myeloid leukemia (AML), gastrointestinal stromal tumor (GIST), and glioma. Crenolanib is an orally bioavailable benzimidazole that selectively and potently inhibits signaling of wild-type and mutant isoforms of class III receptor tyrosine kinases (RTK) FLT3, PDGFR α, and PDGFR β. Unlike most RTK inhibitors, crenolanib is a type I mutant-specific inhibitor that preferentially binds to phosphorylated active kinases with the ‘DFG in’ conformation motif.

Diffuse midline glioma, H3 K27-altered(DMG) is a fatal tumour that arises in midline structures of the brain, most commonly the brainstem, thalamus and spinal cord. When located in the pons it is also known as diffuse intrinsic pontine glioma (DIPG).
An oxygen diffusion-enhancing compound is any substance that increases the availability of oxygen in body tissues by influencing the molecular structure of water in blood plasma and thereby promoting the movement (diffusion) of oxygen through plasma. Oxygen diffusion-enhancing compounds have shown promise in the treatment of conditions associated with hypoxia and ischemia. Such conditions include hemorrhagic shock, myocardial infarction, and stroke.

Zotiraciclib (TG02) is a potent oral spectrum selective kinase inhibitor for the treatment of cancer. It was discovered in Singapore by S*BIO Pte Ltd and falls under the category of small molecule macrocycles. It crosses the blood brain barrier and acts by depleting Myc through the inhibition of cyclin-dependent kinase 9 (CDK9). It is one of a number of CDK inhibitors under investigation; others targeting CDK9 for the treatment of acute myeloid leukemia include alvocidib and atuveciclib. Myc overexpression is a known factor in many cancers, with 80 percent of glioblastomas characterized by this property. Zotiraciclib has been granted orphan drug designation by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the treatment of gliomas.
A cerebroprotectant is a drug that is intended to protect the brain after the onset of acute ischemic stroke. As stroke is the second largest cause of death worldwide and a leading cause of adult disability, over 150 drugs tested in clinical trials to provide cerebroprotection.