Stevens–Johnson syndrome (SJS) is a type of severe skin reaction. Together with toxic epidermal necrolysis (TEN) and Stevens–Johnson/toxic epidermal necrolysis (SJS/TEN) overlap, they are considered febrile mucocutaneous drug reactions and probably part of the same spectrum of disease, with SJS being less severe. Erythema multiforme (EM) is generally considered a separate condition. Early symptoms of SJS include fever and flu-like symptoms. A few days later, the skin begins to blister and peel, forming painful raw areas. Mucous membranes, such as the mouth, are also typically involved. Complications include dehydration, sepsis, pneumonia and multiple organ failure.

Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are involved in a wide range of physiological processes, including stress response, immune response, and regulation of inflammation, carbohydrate metabolism, protein catabolism, blood electrolyte levels, and behavior.

Cushing's syndrome is a collection of signs and symptoms due to prolonged exposure to glucocorticoids such as cortisol. Signs and symptoms may include high blood pressure, abdominal obesity but with thin arms and legs, reddish stretch marks, a round red face due to facial plethora, a fat lump between the shoulders, weak muscles, weak bones, acne, and fragile skin that heals poorly. Women may have more hair and irregular menstruation. Occasionally there may be changes in mood, headaches, and a chronic feeling of tiredness.

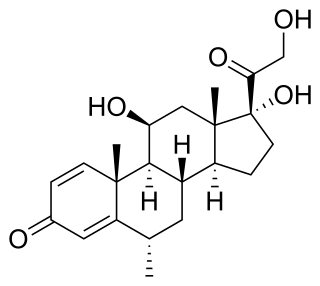
Prednisone is a glucocorticoid medication mostly used to suppress the immune system and decrease inflammation in conditions such as asthma, COPD, and rheumatologic diseases. It is also used to treat high blood calcium due to cancer and adrenal insufficiency along with other steroids. It is taken by mouth.

Granulomatosis with polyangiitis (GPA), also known as Wegener's granulomatosis (WG), after the German physician Friedrich Wegener, is a rare long-term systemic disorder that involves the formation of granulomas and inflammation of blood vessels (vasculitis). It is an autoimmune disease and a form of vasculitis that affects small- and medium-size vessels in many organs but most commonly affects the upper respiratory tract, lungs and kidneys. The signs and symptoms of GPA are highly varied and reflect which organs are supplied by the affected blood vessels. Typical signs and symptoms include nosebleeds, stuffy nose and crustiness of nasal secretions, and inflammation of the uveal layer of the eye. Damage to the heart, lungs and kidneys can be fatal.

Membranous glomerulonephritis (MGN) is a slowly progressive disease of the kidney affecting mostly people between ages of 30 and 50 years, usually white people.
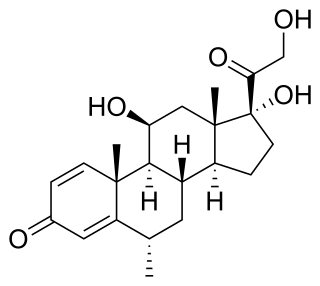
Methylprednisolone is a synthetic glucocorticoid, primarily prescribed for its anti-inflammatory and immunosuppressive effects. It is either used at low doses for chronic illnesses or used concomitantly at high doses during acute flares. Methylprednisolone and its derivatives can be administered orally or parenterally.

Anakinra, sold under the brand name Kineret, is a biopharmaceutical medication used to treat rheumatoid arthritis, cryopyrin-associated periodic syndromes, familial Mediterranean fever, and Still's disease. It is a slightly modified recombinant version of the human interleukin 1 receptor antagonist protein. It is marketed by Swedish Orphan Biovitrum. Anakinra is administered by subcutaneous injection.
Antenatal steroids, also known as antenatal corticosteroids, are medications administered to pregnant women expecting a preterm birth. When administered, these steroids accelerate the maturation of the fetus' lungs, which reduces the likelihood of infant respiratory distress syndrome and infant mortality. The effectiveness of this corticosteroid treatment on humans was first demonstrated in 1972 by Sir Graham Liggins and Ross Howie, during a randomized control trial using betamethasone.
Mixed connective tissue disease, commonly abbreviated as MCTD, is an autoimmune disease characterized by the presence of elevated blood levels of a specific autoantibody, now called anti-U1 ribonucleoprotein (RNP) together with a mix of symptoms of systemic lupus erythematosus (SLE), scleroderma, and polymyositis. The idea behind the "mixed" disease is that this specific autoantibody is also present in other autoimmune diseases such as systemic lupus erythematosus, polymyositis, scleroderma, etc. MCTD was characterized as an individual disease in 1972 by Sharp et al., and the term was introduced by Leroy in 1980.
Steroid-induced osteoporosis is osteoporosis arising from the use of glucocorticoids analogous to Cushing's syndrome but involving mainly the axial skeleton. The synthetic glucocorticoid prescription drug prednisone is a main candidate after prolonged intake. Bisphosphonates are beneficial in reducing the risk of vertebral fractures. Some professional guidelines recommend prophylactic calcium and vitamin D supplementation in patients who take the equivalent of more than 30 mg hydrocortisone, especially when this is in excess of three months. The use of thiazide diuretics, and gonadal hormone replacement has also been recommended, with the use of calcitonin, bisphosphonates, sodium fluoride or anabolic steroids also suggested in refractory cases. Alternate day use may not prevent this complication.
Barraquer–Simons syndrome is a rare form of lipodystrophy, which usually first affects the head, and then spreads to the thorax. It is named for Luis Barraquer Roviralta (1855–1928), a Spanish physician, and Arthur Simons (1879–1942), a German physician. Some evidence links it to LMNB2.
Drug rash with eosinophilia and systemic symptoms or drug reaction with eosinophilia and systemic symptoms (DRESS), also termed drug-induced hypersensitivity syndrome (DIHS), is a rare reaction to certain medications. It involves primarily a widespread skin rash, fever, swollen lymph nodes, and characteristic blood abnormalities such as an abnormally high level of eosinophils, low number of platelets, and increased number of atypical white blood cells (lymphocytes). However, DRESS is often complicated by potentially life-threatening inflammation of internal organs and the syndrome has about a 10% mortality rate. Treatment consists of stopping the offending medication and providing supportive care. Systemic corticosteroids are commonly used as well but no controlled clinical trials have assessed the efficacy of this treatment.
Adult-onset Still's disease (AOSD) is a form of Still's disease, a rare systemic autoinflammatory disease characterized by the classic triad of fevers, joint pain, and a distinctive salmon-colored bumpy rash. The disease is considered a diagnosis of exclusion. Levels of the iron-binding protein ferritin may be extremely elevated with this disorder. AOSD may present in a similar manner to other inflammatory diseases and to autoimmune diseases, which must be ruled out before making the diagnosis.
Topical steroids are the topical forms of corticosteroids. Topical steroids are the most commonly prescribed topical medications for the treatment of rash and eczema. Topical steroids have anti-inflammatory properties and are classified based on their skin vasoconstrictive abilities. There are numerous topical steroid products. All the preparations in each class have the same anti-inflammatory properties but essentially differ in base and price.

Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.

Allopurinol hypersensitivity syndrome(AHS) typically occurs in persons with preexisting kidney failure. Weeks to months after allopurinol is begun, the patient develops a morbilliform eruption or, less commonly, develops one of the far more serious and potentially lethal severe cutaneous adverse reactions viz., the DRESS syndrome, Stevens Johnson syndrome, or toxic epidermal necrolysis. About 1 in 1000 patients receiving allopurinol are affected, and mortality rates have been reported to be between 20% and 25%.
Behçet's disease is recognized as a disease that cause inflammatory perivasculitis, inflammation of the tissue around a blood or lymph vessel, in practically any tissue in the body. Usually, prevalent symptoms include canker sores or ulcers in the mouth and on the genitals, and inflammation in parts of the eye. In addition, patients experience severe headache and papulopustular skin lesions as well. The disease was first described in 1937 by a Turkish dermatologist, Dr. Hulusi Behçet. Behçet's disease is most prevalent in the Middle East and the Far East regions; however, it is rare in America regions.

Chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature (CANDLE) syndrome is an autosomal recessive disorder that presents itself via various autoinflammatory responses throughout the body, multiple types of skin lesions, and recurrent long-term fever symptoms. The current known cause for the disorder is a mutation in the PSMB8 gene or mutations in other closely related genes. The syndrome was first named and classified in March 2010 after four patients were reviewed with similar symptoms. There have been approximately 30 cases reported in the scientific literature as of 2015.
Corticosteroid-induced lipodystrophy (CIL) is a condition of abnormal fat deposition caused by corticosteroid medications. Fat accumulates in the facial area, dorsocervical region, and abdominal area, whereas the thickness of subcutaneous fat in the limbs is decreased. The resulting appearance has been described as "Cushingoid", in relation to the fact that it also occurs in individuals with Cushing's syndrome. The condition is considered by patients to be the most distressing side effect caused by corticosteroids.